More Data Needed to Eliminate the Guesswork In Using Evidence Blocks
The Evidence Blocks developed by the National Comprehensive Cancer Center make up one of the most ambitious attempts so far to incorporate data from multiple platforms to create a resource with broad applicability for the healthcare community.
Robert W. Carlson, MD, CEO of NCCN
Various systems are emerging to help doctors and patients determine whether the anti-cancer medications they are considering will deliver the best value in terms of cost and performance. The Evidence Blocks developed by the National Comprehensive Cancer Center (NCCN) make up one of the most ambitious attempts so far to incorporate data from multiple platforms to create a resource with broad applicability for the healthcare community.
The Evidence Blocks’ multi-dimensional constructs combined with the wealth of science and thought behind the NCCN Guidelines for cancer treatment present an enormous advantage over other value tools in existence, although the difficulty of predicting how a certain disease case will respond to different medications that may make perfection of value tools a far-off goal. For this reason, officials who have been involved in the development of Evidence Blocks acknowledged at the NCCN’s 21st annual meeting in April that much more data need to be gathered and incorporated into the reasoning process that goes into the formulation of these decisionmaking tools. For example, the existence of variables and the subjective nature of some of the ratings given by officials who participate in Evidence Block creation can make it hard for physicians and patients to accept that toxicity ratings of 3 for one therapy and 4 for another in the same disease setting represent an absolutely reliable comparison.
Similarly, the affordability of a drug, although its value in dollars and cents may be a very clear measure, is also highly subjective, given that the high dollar cost of a drug may not be a consideration for a well-heeled or well-insured patient who may be more concerned with toxicity. For example, a professional pianist who fears neuropathy may consider a drug superior that does not cause that side effect.
“The Guidelines are really population-based, and if you’re talking about individuals, you’re talking about hundreds of thousands of individuals throughout the United States,” said Robert W. Carlson, MD, CEO of the NCCN. “Those individuals will have different preferences, different insurance plans, and different co-pays. They’ll have different thresholds for what is expensive or not.”
The NCCN’s Evidence Blocks provide multiple measures of the value of a particular therapy: efficacy, safety, affordability, quality, and consistency of evidence. Each is rated on a scale of 1 to 5. Given that there is likely to be variability among patients in terms of their personal preferences, ages, and relative abilities to tolerate aggressive treatment, the Evidence Blocks must also serve as a starting point for constructive discussion between physician and patient in order to arrive at the optimal therapy, NCCN officials said.
“We’re taking guesses at what patients would want and what it costs us,” agreed Douglas W. Blayney, MD, who served on an ASCO task force that worked to develop a value assessment tool for drugs that remains in its prototype phase. The ASCO Value Framework makes more detailed comparisons of drugs than the Evidence Blocks; however, it only compares drugs that have been evaluated within a particular trial.
All Things Considered, Evidence Blocks Add Value
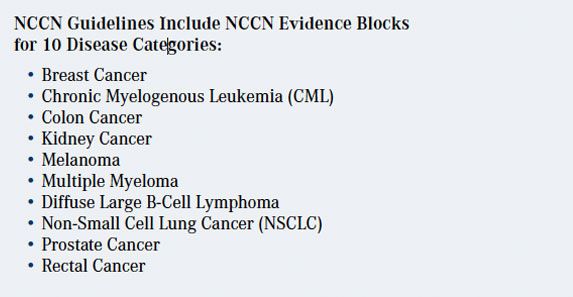
The idiosyncratic nature of treatment notwithstanding, Evidence Blocks represent an important achievement, officials said. Evidence Blocks are now available for recommended treatments in 10 types of cancer, from breast to prostate and from multiple myeloma to chronic myelogenous leukemia, and the list is growing. “We have a commitment that by the end of 2017, we will have Evidence Blocks associated with all systemic therapy guidelines, and we will be moving to include Evidence Blocks for radiation oncology, diagnostics, and surgical oncology procedures in the future,” Carlson said. Carlson is emphatic that Evidence Blocks already constitute a sound basis for value decisions in the physician’s office. Eric Jonasch, MD, of The University of Texas MD Anderson Cancer Center, who gave a presentation on the use of Evidence Blocks in distinguishing the relative merits of different therapies in renal cell carcinoma, agreed with Carlson that, despite the lack of precise data on relative drug performance, Evidence Blocks do serve as valuable directional instruments for treatment decisions.
“The Evidence Blocks are beginning to create what I would call a succinct interpretation of the data which can begin to generate a dialog between the patients and the treatment teams,” he said. “The other thing that’s very clear is that ongoing refinement of these Evidence Blocks is necessary. This is something that we’re beginning to get our heads around: what defines quality of response? What defines relative toxicity? When it comes to affordability, what does affordability mean? And affordability for whom, and how do we measure that? How we improve that for the various agents that are available for renal cell carcinoma, I think, is a critical thing that we need to talk about,” Jonasch said.




