Payer Payment Delays Are Escalating
As increasingly pricey therapies come on the market, payers have grown more cautious about issuing payment approvals.
Ray Page, DO, PhD

Ray Page, DO, PhD
When coding and billing consultant Roberta Buell mentions that payers are taking dramatically longer to pay claims, oncology practice administrators nod in agreement. At Carolina Blood and Cancer Care, Kashyap Patel, MD, who attended a recent public address1 by Buell, said that it is now taking up to 3 months to get paid, up from maximum delays of a month a few years ago. And Ray Page, DO, PhD, said that the constant delays and treatment denials he has seen at his Texas-based practice, the Center for Cancer & Blood Disorders, have caused losses, led to physician burnout, and adversely affected patients’ treatment regimens.
Both men say their practices are doing all they can, but it’s still a struggle to stay on top of the revenue cycle. “We noticed such a dramatic change in payment times this year that we thought we needed to bring it up with the physician board,” Page said. “We’re coming around for the next cycle of drugs, and we haven’t gotten paid for the first one. And in some cases, we even get into a third cycle of treatment without being paid for the first. That’s a huge financial outlay that practices can’t afford.”
As increasingly pricey therapies come on the market, payers have grown more cautious about issuing payment approvals. Documentation requirements are stiffer, practices must traverse more gateways during the approvals process, and a lot more explaining must be done to convince a payer that therapy choices made by doctors are medically necessary (Table).
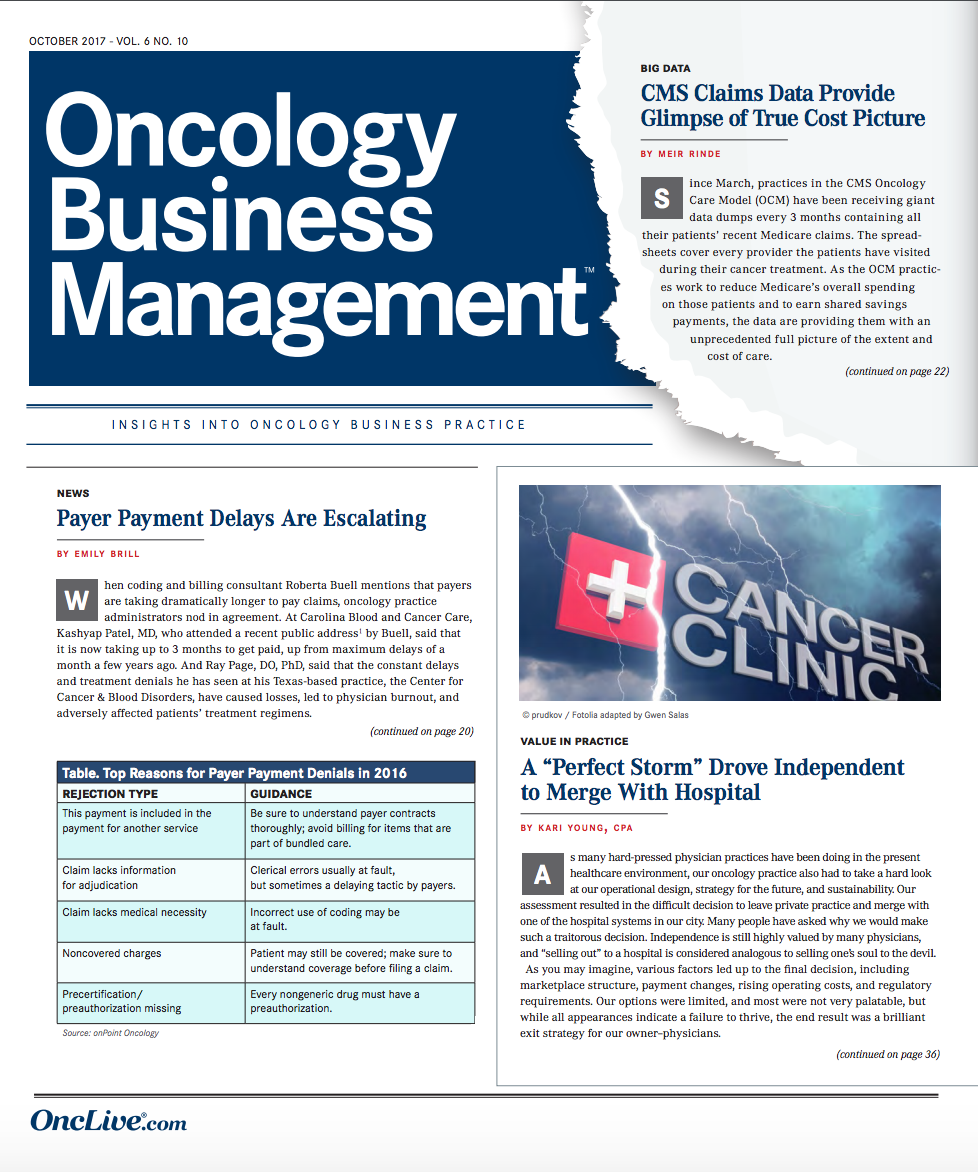
Table. Top Reasons for Payer Payment Denials in 2016
The majority of Medicare Part B drug claims are generally paid within a month, according to Buell, of onPoint Oncology in Hudson, Ohio. Her review of focalPoint 2016 data from 165 cancer centers across the country found that 63% of accounts receivable claims were less than 1 month old; 18.6%, between 1 and 2 months old; 4.51%, up to 3 months old; 2.51%, up to 120 days old; and 11.32%, up to 4 months old.
Some payers were singled out by Buell for taking up to 3 months to pay intravenous drug claims, although she praised others for being especially good about paying these claims. Several payers were asked to comment for this article, including Mutual of Omaha, LaSalle Medical Associates, Nevada Blue Shield, Delaware Blue Cross, and New Mexico Blue Cross. None responded. Buell’s data indicated that each took an average of 2 months or longer to pay claims for injectable drugs.
When it comes to types of service, the payment rates look better: among payers in general, evaluation and management claims required an average of 18 days for payment in 2016; imaging, 37 days; radiation, 28 days; and drugs, 36 days. Practices have responded to the changes in payment policy by beefing up staff dedicated to handling claims and ensuring payment. Page said that his practice has increased its preauthorization staff from 2 to 5 people: “a 150% increase in staffing—folks who do nothing but preauthorization.” Patel said his North Carolina practice recently increased its preauthorization staff as well, from 1 to 2. A few years ago, his practice didn’t employ anyone whose sole job function was securing preauthorizations for treatment.
“One of the employees started on the front desk, and now this is all she does. And we just hired another employee at the other office just to ensure we don’t drop the ball on anything,” Patel said. He said employees need to obtain preauthorization for drugs, especially high-priced ones, because of the possibility that payers will refuse to pay. “My blanket observation is: If the medicine is expensive, they will always give us a hard time, no matter what.”
Page said that hiring multiple people to handle preauthorization isn’t an ideal long-term solution. First, there’s the cost; and, second, securing preauthorization for a treatment doesn’t guarantee that the treatment will be paid for. He dreams of a world where the revenue cycle is fully automated, with physicians using their electronic health record system and evidence-based treatment pathways to show payers why a treatment is necessary, rather than “burning up our fax machines,” then waiting weeks for a response.
1. Advise physicians to be meticulous in their record keeping because payers are asking for more documentation.
He and Patel, along with Buell and Teri Guidi, CEO of Oncology Management Consulting Group in Tampa, Florida, have some advice for improving the flow of the revenue cycle.Getting the ICD-102 medical codes right is important, but simply ensuring that a code is accurate may not be enough to guarantee prompt payment, Page said. “You may submit an ICD-10 code that says a patient has metastatic breast cancer. But for the payers, the ICD-10 code is not good enough—they want the whole chart,” he said.
Thus, he advises physicians to stay on top of their charting. “If the payer is asking for the complete consultation to make the decision, and maybe our doctor hasn’t dictated the consultation or it’s being transcribed, or maybe there’s a delay in getting information on the chart, then that amounts to a potential delay in payment,” Page said.
2. Negotiate the payer contracts so that payers must respond to claims promptly.
3. Hire additional staff.
Guidi advises practices to “document, document, document.” Each billable code should be submitted with a physician order, documentation of medical necessity, and documentation of physician involvement, she said. Buell recommends double-checking patients’ charts after coding to ensure that every drug has been accounted for and that the codes are correct for each drug. She advises practices to be extra careful about selecting the correct diagnosis codes for leukemia and non-Hodgkin lymphoma, as physicians tend to take notes in a way that complicates the process of choosing an ICD-10 code for those diagnoses.Guidi, who advises oncology practices of all sizes and hospital cancer-care wings, tells her clients to hold payers accountable for their contractual promises. “Most payer contracts have ‘timely filing’ terms, which specify how long after the date of service you can file a claim, a corrected claim, or an appeal. A lot of payers allow 6 months,” she said. “The thing is that a lot of payer contracts don’t say anything about how quickly they have to respond to a filed claim. If there’s no language in there about that, they can wait until the last minute, and then it’s too late to refile.”Although hiring more employees to handle preauthorization or serve as financial counselors may be inferior to moving toward automation, Patel and Guidi said they have seen hiring solutions that worked for certain practices.
Drug companies give practices a discount if they pay for drugs quickly after receiving them, and that discount adds up. Patel said additional staff can pay for themselves if they are good at making this process flow smoothly. “If we’re able to pay the bills for drugs on time—within 7 days of buying them—I may be able to create savings good enough to allow for an extra employee,” Patel said.
Although the expense of hiring additional workers may be too much for smaller practices, Patel said that if they can swing it, they should do it. For physicians in practices without administrators, “the time we would spend caring for the patient is spent trying to get past these bureaucratic hurdles that we face,” he said. Hiring an administrator can alleviate that burden somewhat. For practices with bigger budgets, Guidi advises hiring a financial counselor.
4. Intervene early enough in the revenue cycle to avoid denials on the back end.
Financial counselors can help patients enroll in insurance programs, secure help from co-pay assistance programs, and facilitate drug replacements and payment from foundations. “They definitely will pay for themselves, unless the practice is already running like a fine-tuned machine,” she said.This has become something of a mantra among oncology consultants. Guidi recommends taking the following actions on the front end:
- Ensure that staff have an up-to-date understanding of payers’ rules.
- If possible, hard-wire rule checks into your systems.
- Verify insurance at every visit, or at least monthly.
- Obtain and check preauthorizations or precertifications for every visit.
- Use all available drug-replacement options.
- In the case of particularly difficult payers, consider submitting all prior documentation with new claims.
Guidi said that practices are more sensitive to revenue flow and are likely to chase down potential funds. “Everybody in the practice lives and dies by the practice’s finances,” she said. “Everybody in a hospital billing department does not.” Practices are less likely to let a denial slip by, whereas a hospital may forgo chasing after a $250 care denial when there’s been a $25,000 care denial.
Buell said practices should remember that the more work that is done up front to ensure payment, the more money the practice will receive in the long run. She recommended that practices provide incentives for people involved in revenue collections—“pay, paid time off, pizza, etc”—and track progress when it comes to care denials. “Benchmark yourself against local and national statistics,” she said. “Invest in systems to track, work, and report denials and measure improvement on an ongoing basis. Don’t start and stop.”
Patel and Page acknowledge that instituting best practices for revenue cycle management can help, but at the end of the day, payers still delay payment—and that wears on practices and their patients. “A lot of times, these [payment] delays result in delays restaging a diagnosis,” Page said. “It’s hard and frustrating…I’m passionately concerned about my patients, and when I see things that are detrimental to them, it really gets me twisted. And we’ve got a whole village of people in my office trying to remedy these situations. One of our preauthorization staff spends a good part of the workday on hold. The process is not efficient or modern. It’s archaic.”
One of the toughest things to get used to is having payers use their leverage to influence the clinical decision process more than ever before. “When you’re in a position of power and accountability—I’m totally accountable for my patients—and you have these massive administrative burdens,” Page said, “and you’re dealing with payers making decisions for you that you think aren’t in the best interest of the patient—when you put all that together, you can get burned out.”
References
- Buell B. Revenue cycle: state of the state. Presented at: Community Oncology Alliance 2017 conference. http://coaconference.org/2017Presentations/f/genbiz/ Fri-1015am-The-Coding-Mistress-Actionable.pdf. Accessed August 17, 2017.
- ICD-10 indicates10th revision of the International Statistical Classification of Diseases and Related Health Problems.