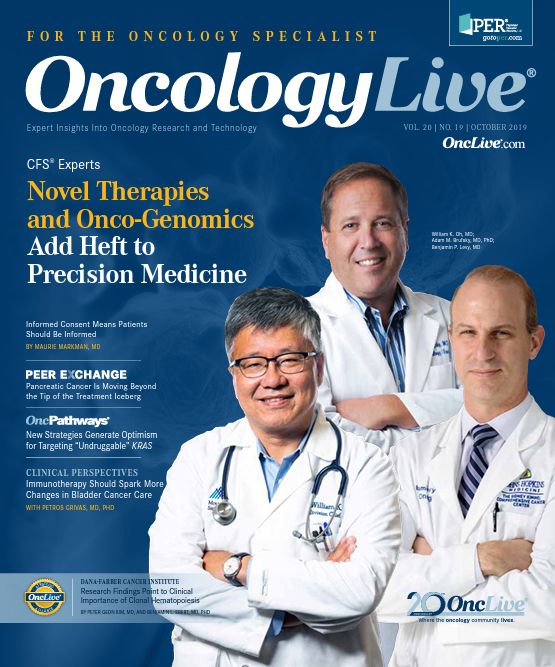
Research Findings Point to Clinical Importance of Clonal Hematopoiesis
Although clonal hematopoiesis of indeterminate potential is recognized as a risk factor for developing hematological neoplasms, a growing body of evidence points to its potential significance in broader clinical scenarios.
Peter Geon Kim, MD
Postdoctoral fellow
Department of Medicine
Dana-Farber Cancer Institute
Boston, Massachusetts

Benjamin L. Ebert, MD, PhD
George P. Canellos, MD, and Jean S. Canellos Professor of Medicine
Harvard Medical School
Chair, Department of Medical Oncology
Dana-Farber Cancer Institute
Boston, Massachusetts
Although clonal hematopoiesis of indeterminate potential (CHIP) is recognized as a risk factor for developing hematological neoplasms, a growing body of evidence points to its potential significance in broader clinical scenarios.
CHIP refers to the presence of somatic mutations identified via clinical sequencing of hematopoietic cells and occurs in the absence of cytopenias; it is a premalignant state associated with cardiovascular disease and other adverse outcomes.1-3 National Comprehensive Cancer Network guidelines for myelodysplastic syndrome (MDS) recommend that individuals with CHIP be followed every 6 months or more frequently based on clinical expertise.
A typical sequencing report may reveal genes commonly mutated in myeloid malignancies such as TET2, DNMT3A, and ASXL1, especially in individuals older than 60 years.1,2 Individuals with prior exposure to chemotherapy have an increased prevalence of TP53 and PPM1D mutations.4,5 CHIP is defined with a variant allele fraction (VAF) cutoff of 2%, but many of the clinical consequences of CHIP occur in individuals with a VAF >10%.
The rate of progression from CHIP to hematological malignancy is approximately 0.5% to 1% per year, similar to that of other premalignant states.6 When patients with CHIP develop cytopenias, the condition is termed clonal cytopenia of undetermined significance (CCUS), and these individuals have a higher rate of progression to MDS.7 Patients with CCUS can be risk-stratified further based on mutational burden (VAF ≥10% or >1 mutation), or co-mutation with a spliceosome gene such as SF3B1, SRSF2, and U2AF1.
Cardiovascular Link and Immunity
CHIP is implicated in the development of coronary artery disease and ischemic heart failure9,10 via the expansion of inflammatory macrophages. Therefore, cardiovascular risk modification should be incorporated into routine clinic visits with these patients. Clonal hematopoiesis can coexist in the setting of inflammatory conditions such as rheumatoid arthritis (RA),11 and population-level data suggest that patients with MDS or acute myeloid leukemia have a 1.7-fold increased risk of autoimmune conditions.12
Whether specific clonal mutations are associated with a particular immune response or condition remains to be determined, and expansion of the sequencing panel beyond myeloid-specific genes may yield additional insight into specific interactions with adaptive immunity. An interesting example of this phenomenon is the STAT3 mutation in individuals with T-cell large granular lymphocytic leukemia, which is lymphocyte-specific and significantly associated with RA.13
After hematopoietic stem cell transplant, CHIP has become an important consideration for prognostication and diagnosis. In the setting of autologous stem cell transplants for lymphoma, the detection of CHIP is associated with inferior survival and increased therapy-related myeloid neoplasms.5 In allogeneic stem cell transplantation, donor-derived CHIP can lead to progressive cytopenias and hematopoietic neoplasms, which pose challenges when determining the cause of relapse.14
Additionally, donor CHIP is associated with increased cumulative incidence of chronic graft-versus-host disease and a lower relapse rate, again implying complex immune regulation that is not currently well understood.15 These variables could, in the future, factor into donor screening for transplantation and may offer clues to enhanced immune surveillance that is observed post transplant.
Solid Tumor Implications
Beyond hematology, next-generation sequencing is increasingly incorporated into guidelines for the management of solid malignancies. Many of these sequencing panels commonly include mutations described in CHIP. It is important to be cognizant of this because mutations detected in bulk sequencing could represent mutations in the blood.16
For example, when the JAK2 V617F mutation is detected as CHIP, it is associated with increased incidence of venous thrombosis.17 Individuals with both solid malignancies and JAK2 CHIP can be at high risk for venous thromboembolism and should be referred to an appropriate specialist. At Dana-Farber Cancer Institute, we recently initiated a clinic for dealing with these referrals for hematologic premalignancies so that such blood mutations can be confirmed and their risk factors appropriately managed.
What was thought to be simply a risk factor for developing hematological neoplasms has now assumed a critical role in a variety of conditions. CHIP is implicated in cardiovascular disease, outcomes after hematopoietic transplant, and beyond. In addition to increasing awareness and appropriate risk modifications, increasing focus on the role of specific mutations and immune regulation will help us understand how these mutations can be harnessed for therapeutic benefit.
References
- Genovese G, Kähler AK, Handsaker RE, et al. Clonal hematopoiesis and blood-cancer risk inferred from blood DNA sequence. N Engl J Med. 2014;371(26):2477-2487. doi: 10.1056/NEJMoa1409405.
- Jaiswal S, Fontanillas P, Flannick J, et al. Age-related clonal hematopoiesis associated with adverse outcomes. N Engl J Med. 2014;371(26):2488-2498. doi: 10.1056/NEJMoa1408617.
- Jaiswal S, Natarajan P, Silver AJ, et al. Clonal hematopoiesis and risk of atherosclerotic cardiovascular disease. N Engl J Med. 2017;377(2):111-121. doi: 10.1056/NEJMoa1701719.
- Coombs CC, Zehir A, Devlin SM, et al. Therapy-related clonal hematopoiesis in patients with non-hematologic cancers is common and associated with adverse clinical outcomes. Cell Stem Cell. 2017;21(3):374-382.e4. doi: 10.1016/j.stem.2017.07.010.
- Gibson CJ, Lindsley RC, Tchekmedyian V, et al. Clonal hematopoiesis associated with adverse outcomes after autologous stem-cell transplantation for lymphoma. J Clin Oncol. 2017;35(14):1598-1605. doi: 10.1200/JCO.2016.71.6712.
- Steensma DP, Bejar R, Jaiswal S, et al. Clonal hematopoiesis of indeterminate potential and its distinction from myelodysplastic syndromes. Blood. 2015;126(1):9-16. doi: 10.1182/blood-2015-03-631747.
- Kwok B, Hall JM, Witte JS, et al. MDS-associated somatic mutations and clonal hematopoiesis are common in idiopathic cytopenias of undetermined significance. Blood. 2015;126(21):2355-2361. doi: 10.1182/blood-2015-08-667063.
- Fuster JJ, MacLauchlan S, Zuriaga MA, et al. Clonal hematopoiesis associated with TET2 deficiency accelerates atherosclerosis development in mice. Science. 2017;355(6327):842-847. doi: 10.1126/science.aag1381.
- Dorsheimer L, Assmus B, Rasper T, et al. Association of mutations contributing to clonal hematopoiesis with prognosis in chronic ischemic heart failure. JAMA Cardiol. 2019;4(1):25-33. doi: 10.1001/jamacardio.2018.3965.
- Sano S, Oshima K, Wang Y, et al. Tet2-mediated clonal hematopoiesis accelerates heart failure through a mechanism involving the IL-1 β/NLRP3 inflammasome. J Am Coll Cardiol. 2018;71(8):875-886. doi: 10.1016/j.jacc.2017.12.037.
- Savola P, Lundgren S, Keranen MAI, et al. Clonal hematopoiesis in patients with rheumatoid arthritis. Blood Cancer J. 2018;8(8):69. doi: 10.1038/s41408-018-0107-2.
- Kristinsson SY, Bjorkholm M, Hultcrantz M, Derolf AR, Landgren O, Goldin LR. Chronic immune stimulation might act as a trigger for the development of acute myeloid leukemia or myelodysplastic syndromes. J Clin Oncol. 2011;29(21):2897-2903. doi: 10.1200/JCO.2011.34.8540.
- Rajala HL, Olson T, Clemente MJ, et al. The analysis of clonal diversity and therapy responses using STAT3 mutations as a molecular marker in large granular lymphocytic leukemia. Haematologica. 2015;100(1):91-99. doi: 10.3324/haematol.2014.113142.
- Gibson CJ, Kennedy JA, Nikiforow S, et al. Donor-engrafted CHIP is common among stem cell transplant recipients with unexplained cytopenias. Blood. 2017;130(1):91-94. doi: 10.1182/blood-2017-01-764951.
- Frick M, Chan W, Arends CM, et al. Role of donor clonal hematopoiesis in allogeneic hematopoietic stem-cell transplantation. J Clin Oncol. 2019;37(5):375-385. doi: 10.1200/JCO.2018.79.2184.
- Ptashkin RN, Mandelker DL, Coombs CC, et al. Prevalence of clonal hematopoiesis mutations in tumor-only clinical genomic profiling of solid tumors. JAMA Oncol. 2018;4(11):1589-1593. doi: 10.1001/jamaoncol.2018.2297.
- Wolach O, Sellar RS, Martinod K, et al. Increased neutrophil extracellular trap formation promotes thrombosis in myeloproliferative neoplasms. Sci Transl Med. 2018;10(436). doi: 10.1126/scitranslmed.aan8292.