New Therapeutic Era Sparks Fresh Questions About Nephrectomy in RCC
Although fewer patients are undergoing cytoreductive nephrectomy as systemic treatments for renal cell carcinoma improve, the modality still has a vital role to play in the treatment paradigm—even in the modern age of immune checkpoint inhibitors.
Brian Shuch, MD

Brian Shuch, MD
Although fewer patients are undergoing cytoreductive nephrectomy (CN) as systemic treatments for renal cell carcinoma (RCC) improve, the modality still has a vital role to play in the treatment paradigm-even in the modern age of immune checkpoint inhibitors (ICIs), said Brian Shuch, MD.
Early results from ICI trials demonstrate safety and efficacy in patients with RCC, and ongoing trials are looking into the optimal use for neoadjuvant treatment with preoperative immunotherapy. Nonetheless, Shuch, director of the Institute of Urologic Oncology Kidney Cancer Program and the Henry Alvin and Carrie L. Meinhardt Endowed Chair for Kidney Research at the University of California, Los Angeles, said surgery is still likely to play a role in the treatment of RCC now and in the future.
"For many different eras, surgery has been relevant," he said. "Why would that change now? We just need to find the right patients, the right timing."
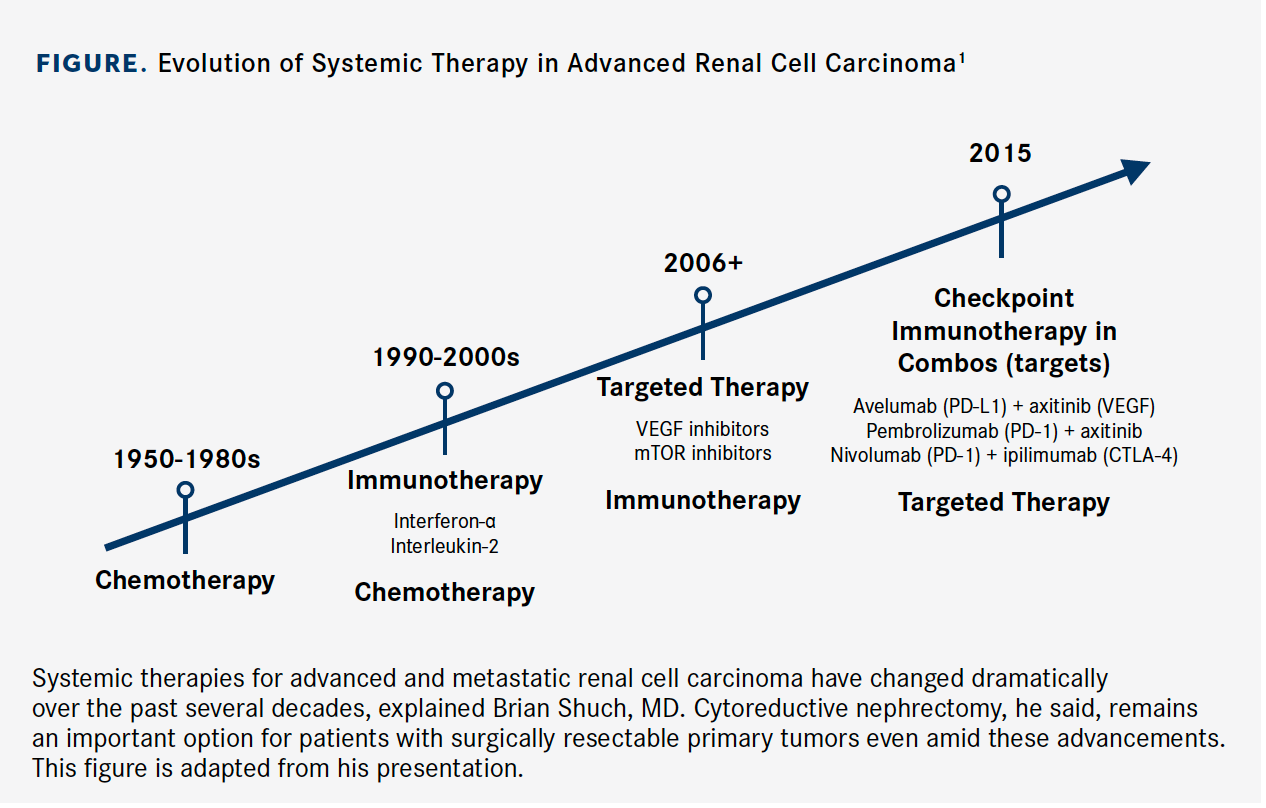
Shuch discussed the evolving role of surgery in advanced RCC in the context of changes in systemic therapy options (Figure) during the New York GU 13th Annual Interdisciplinary Prostate Cancer Congress® and Other Genitourinary Malignancies conference.1
Anti-VEGF Agents Induce Responses
In the cytokine era of the 1990s, clinical trial data clearly supported the superiority of CN followed by interferon-α over interferon- α alone and that approach became a standard of care for treating de novo metastatic RCC, Shuch said.
Patients with 3 or fewer preoperative risk factors have better median overall survival (OS) after CN than patients who have 4 or more risk factors (22.7 vs 12.2 months). The latter group does not appear to benefit from the surgery.2
However, cytokines rarely induce a response in the primary tumor, but neoadjuvant treatment with VEGF-targeting tyrosine kinase inhibitors such as sunitinib (Sutent), pazopanib (Votrient), and axitinib (Inlyta) commonly results in tumor shrinkage, which suggested a potential change in surgical approach, Shuch said.
In 2019, Bossé et al published data from a pooled analysis of 12 phase 2/3 clinical trials of patients with metastatic RCC who received systemic therapy with tyrosine kinase inhibitors from 2003 to 2013. Data from patients with 1 target lesion in the kidney were identified as having theirprimary tumor in place (N = 565) and were evaluated. The study population included 461 (82%) patients who had not undergone treatment. Half of the patients had received first-line VEGF-targeted therapy, and 39% were poor risk as determined by International Metastatic RCC Database Consortium (IMDC) criteria. The primary end point was objective response rate (ORR) in the primary tumor.3
The ORR in the primary tumor was 19% (95% CI, 16%-23%) for patients who received first-line therapy of any type compared with 28% (95% CI, 22%-33%) for those who received VEGF inhibitors in the first line and 23% (95% CI, 19%-28%) for those treated with VEGF-targeted therapy in any line. The ORR was 9% (95% CI, 5%-13%) for patients with poor risk and 20% (95% CI, 15%-27%) for those with intermediate risk.
Shuch noted that tumors shrank in the patients assigned to VEGF inhibitors, albeit slowly, and the response was mild. At 6 weeks, 60% of patients had a 7% mean reduction in tumor size. That number increased to 12% at 18 weeks and 18% at 24 weeks.
Figure. Evolution of Systemic Therapy in Advanced Renal Cell Carcinoma1 (Click to Enlarge)
CN Remains Benefical in the Right Population
Based on data from the SURTIME trial published in 2019, delayed CN does not appear to affect progression-free survival but may improve OS by eliminating patients who are harmed by surgery.4
SURTIME (NCT0109942) was a randomized clinical phase 3 trial comparing immediate CN followed by sunitinib versus 3 cycles of sunitinib followed by CN and sunitinib. Recruitment was poor—investigators enrolled only 99 out of a planned 458 patients—so the independent data monitoring committee endorsed reporting the intention-to-treat 28-week progressionfree rate instead.
Fifty patients were assigned to immediate nephrectomy, whereas surgery was deferred in 49 patients. In the deferred arm, 29% of patients never progressed to surgery.
At 28 weeks, the progression-free rate was 42% in the immediate surgery arm versus 43% in the delayed surgery arm. In the intention-to-treat population, the median OS was 15.0 months (95% CI, 9.3-29.5) in the immediate CN arm compared with 32.4 months (95% CI, 14.5- 65.3) in the deferred arm (HR, 0.57; 95% CI, 0.34-0.95; P = .032).
Choueiri et al published a retrospective review in 2011 showing that patients with metastatic RCC who had not received VEGF therapy had dramatic improvement in OS with CN compared with those who did not undergo CN (19.8 vs 9.4 months; HR, 0.44; 95% CI, 0.32-0.59; P <.01). However, subgroup analyses stratified for favorable-, intermediate-, or poor-risk criteria showed that patients with poor risk only derived marginal benefit (P = .06). Overall, patients who were poor surgical candidates had poor outcomes after surgery.5
In the phase 3 CARMENA trial (NCT00930033), investigators randomized 450 patients with metastatic clear cell RCC; 226 underwent CN followed by sunitinib, and 224 were assigned to sunitinib alone. In the surgery group, patients started sunitinib between 3 to 6 weeks after surgery to allow time for recovery.
Interim findings published in 2018 showed that sunitinib monotherapy was noninferior to CN followed by sunitinib. The HR for death with sunitinib monotherapy was 0.89 (95% CI, 0.71-1.10). Furthermore, monotherapy conferred a 4.5-month advantage in median OS (18.4 vs 13.9 months). Between those results and the findings from Choueiri et al, some experts wondered whether the use of CN was coming to an end.6
However, Shuch said the study participants may not represent patients generally considered for surgery. He noted that 44.4% of those in the nephrectomy-sunitinib group were in the poor-risk category. He added that the median OS of 13.9 months in the surgery arm is "very low" and similar to data from EORTC/SWOG trials published before the availability of effective systemic therapies.
"This just means to me that we’re comparing different patient populations," Shuch said. "Our therapy now is better and if survival hasn’t improved, we’re just looking at a much sicker cohort. In the series of modern cytoreductive nephrectomies with carefully selected patients, we’re looking at a median OS of 15 to 24 months, so this seems to be much worse."
Final results from the CARMENA trial were presented at the 2019 American Society of Clinical Oncology Annual Meeting. In the intermediate-risk group, individuals whose only risk factor was the time from diagnosis to metastatic disease of less than 12 months— a cohort that did not have hemoglobin levels below the lower limit of normal or calcium or neutrophil levels above the upper limit of normal—the median OS was 25.2 months (95% CI, 19.6-35.4) for sunitinib alone versus 31.4 months (95% CI, 17.3-45.5) in the surgery group (HR, 1.29; 95% CI, 0.85-1.98; P = .232). In patients who had 2 risk factors, OS was superior in the sunitinib-alone arm (31.2 vs 17.6 months; HR, 0.63; 95% CI, 0.44- 0.97; P = .033).7
Among the 40 (18%) patients who crossed over to the surgery arm, the median OS was 48.5 months compared with 15.7 months (HR, 0.34; 95% CI, 0.22-0.54) for those who did not undergo surgery.
"The updated conclusions show that [sunitinib], in this poor-risk population, is still not inferior," Shuch said. "CARMENA shows that, in [poor-prognosis] patients who should not have had surgery, surgery is really not helpful."
Trials Explore Surgery in ICI Era
At present, there are 3 ICIs approved to treat patients with advanced RCC: (1) the PD-1 inhibitor nivolumab (Opdivo) as a single-agent treatment after prior antiangiogenic therapy and in combination with the CTLA-4 inhibitor ipilimumab (Yervoy) for previously untreated patients with intermediate- or poor-risk disease; (2) the PD-1 inhibitor pembrolizumab (Keytruda) in combination with axitinib as a firstline treatment; and (3) the PD-L1 inhibitor avelumab (Bavencio) in combination with axitinib as first-line therapy.
ICIs are more potent and better tolerated than other systemic therapies, Shuch said. Early study findings suggest that the adverse events from ICIs are minimal and that CN can be safely conducted in patients who have received these agents.
In a pilot study (NCT02210117), patients with metastatic RCC who had not received prior ICI and anti-VEGF therapy were randomized to receive nivolumab, nivolumab plus the VEGF inhibitor bevacizumab (Avastin), or nivolumab plus ipilimumab, followed by CN, metastasectomy, or biopsy; and subsequent nivolumab maintenance therapy for up to 2 years.
In 12-week findings, investigators observed a best overall response, including complete and partial responses, of 54% among patients in the nivolumab arm (n = 28), 48% in the nivolumab/bevacizumab arm (n = 40), and 41% in the nivolumab/ipilimumab arm (n = 29). Shuch added that the safety profile was acceptable in the perioperative setting.8
In findings reported at the 2020 Genitourinary Cancers Symposium, investigators with the IMDC conducted a retrospective analysis of patients diagnosed with de novo metastatic RCC who started first-line systemic therapy with ICIs or targeted therapy from 2009 to 2019 (N = 4639). Most patients (62%) underwent CN.9
The findings demonstrated that patients who underwent CN experienced improved median OS compared with those who did not have CN, respectively, both with targeted therapies (26.5 vs 10.3 months; HR, 0.48; 95% CI, 0.45-0.52; P <.0001) and with ICIs (53.6 vs 21.4 months; HR, 0.44; 95% CI, 0.30-0.64; P <.0001).
Investigators concluded that the benefits observed with CN appear similar in the targeted therapy and ICIs eras but that patient selection remains important.
Two ongoing trials, PROSPER RCC (NCT03055013) and NORDIC-SUN (NCT03977571), will help to further clarify the role of ICIs and CN in patients with RCC. The phase 3 PROSPER trial, with an estimated enrollment of 805 participants, is randomizing patients to receive perioperative nivolumab or observation in advance of partial or radical nephrectomy. NORDICSUN, also a phase 3 trial, will evaluate initial treatment with nivolumab plus ipilimumab followed by CN in patients with 3 or fewer IMDC risk features or maintenance nivolumab in those with more than 3 risk features.
References
- Shuch B. Evolving therapeutic strategies in renal cell carcinoma: nephrectomy vs no nephrectomy. Presented at: 13th Annual Interdisciplinary Prostate Cancer Congress® and Other Genitourinary Malignancies hosted by Physicians’ Education Resource®, LLC (PER®); March 13-14, 2020; New York, NY.
- Culp SH, Tannir NM, Abel EJ, et al. Can we better select patients with metastatic renal cell carcinoma for cytoreductive nephrectomy? Cancer. 2010;116(14):3378-3388. doi: 10.1002/cncr.25046
- Bossé D, Lin X, Simantov R, et al. Response of primary renal cell carcinoma to systemic therapy. Eur Urol. 2019;76(6):852-860. doi: 10.1016/j.eururo.2019.08.035
- Bex A, Mulders P, Jewett M, et al. Comparison of immediate vs deferred cytoreductive nephrectomy in patients with synchronous metastatic renal cell carcinoma receiving sunitinib: the SURTIME randomized clinical trial [erratum in JAMA Oncol. 2029;5(2):271]. JAMA Oncol. 2019;5(2):164-170. doi: 10.1001/jamaoncol.2018.5543
- Choueiri TK, Xie W, Kollmannsberger C, et al. The impact of cytoreductive nephrectomy on survival of patients with metastatic renal cell carcinoma receiving vascular endothelial growth factor targeted therapy. J Urol. 2011;185(1):60-66. doi: 10.1016/j.juro.2010.09.012
- Méjean A, Ravaud A, Thezenas S, et al. Sunitinib alone or after nephrectomy in metastatic renal-cell carcinoma. N Engl J Med. 2018;379(5):417-427. doi: 10.1056/NEJMoa1803675
- Méjean A, Thezenas S, Chevreau C, et al. Cytoreductive nephrectomy (CN) in metastatic renal cancer (mRCC): update on Carmena trial with focus on intermediate IMDC-risk population. J Clin Oncol. 37, 2019 (suppl; abstr 4508).
- Gao J, Karam JA, Tannir NM, et al. A pilot randomized study evaluating nivolumab (nivo) or nivo + bevacizumab (bev) or nivo + ipilimumab (ipi) in patients with metastatic renal cell carcinoma (MRCC) eligible for cytoreductive nephrectomy (CN), metastasectomy (MS) or post-treatment biopsy (Bx). J Clin Oncol. 2018;36(suppl; abstr 4520). doi: 10.1200/JCO.2018.36.15_suppl.4520
- Bakouny Z, Xie W, Dudani S, et al. Cytoreductive nephrectomy (CN) for metastatic renal cell carcinoma (mRCC) treated with immune checkpoint inhibitors (ICI) or targeted therapy (TT): a propensity score-based analysis. J Clin Oncol. 2020; 38(suppl 6; abstr 608). meetinglibrary.asco.org/record/184115/abstract
"You don’t give it and the tumors shrink in a week or 2," he said. “We’re talking over 12 to 24 weeks of therapy where you get some effects—not really enough to change surgical approach."