Trastuzumab Duocarmazine Active in HER2-Positive Breast Cancer
The HER2-targeting antibody-drug conjugate (vic-)trastuzumab duocarmazine (SYD985) showed promising clinical activity in heavily-pretreated women with metastatic breast cancer.
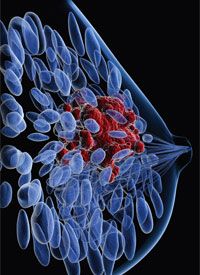
breast cancer
The HER2-targeting antibody-drug conjugate (vic-)trastuzumab duocarmazine (SYD985) showed promising clinical activity in heavily-pretreated women with metastatic breast cancer, according to results from a phase I expansion cohort presented at the 2018 ASCO Annual Meeting.
The objective response rate (ORR) was 33% (16/48) among evaluable patients with HER2-positive disease, including 29% (11/38), among those who had prior T-DM1 (ado-trastuzumab emtansine; Kadcyla). The ORR was 27% (8/30) among evaluable patients with HER2-low/hormone receptor (HR)-positive disease, and 40% (6/15) for those with triple-negative disease. All responses across these subgroups were partial responses.
The median progression-free survival (PFS) was 9.4 months (95% CI, 4.5-12.4) overall in the HER2-positive group, and 8.3 months (95% CI, 4.1-15.0) among those in the group with prior T-DM1. The median PFS was 4.1 months (95% CI, 2.4-5.4) and 4.4 months (95% CI, 1.0-7.1) in the HER2-low/HR-positive and triple-negative arms, respectively.
At the May 1, 2018, data cutoff, 8 patients with HER2-positive disease had received treatment for >1 year, 6 of whom previously received T-DM1 in the metastatic setting. Four patients from across the entire metastatic breast cancer cohort remained on treatment at the cutoff.
Overall, investigators on the phase I study recruited 99 women with heavily-pretreated metastatic breast cancer at 15 sites in Belgium, the Netherlands, the United Kingdom, and Spain. Patients who had gastric, endometrial, or urothelial cancers with at least HER2 immunohistochemistry 1+ expression and who were refractory to standard therapy were also eligible for inclusion in the expansion cohort.
The data presented at ASCO focused on women with metastatic breast cancer. The median age was 54 years (range, 30-80) in the HER2-positive cohort, and 53 years in both the HER2-low/HR-positive (range, 35-74), and triple-negative (range, 35-70) cohorts.
The median number of prior therapies in the HER2-positive group was 6 (range, 1-21), 6 (range, 2-10) in the HER2-low/HR-positive group, and 6 (range, 3-7) in the triple-negative group. Ninety-two percent, 81%, and 65% of patients in the 3 arms, respectively, had received ≥4 prior treatment regimens.
Forty-six (92%) of 50 patients in the HER2-positive group received prior trastuzumab and 40 (80%) received prior T-DM1. In the HER2-low/HR-positive group, 5 (16%) of 32 patients received prior trastuzumab and 2 (6%) received prior T-DM1, while 1 (6%) of 17 patients in the triple-negative arm received prior trastuzumab and none had received T-DM1.
Seventeen patients from the HER2-positive group and all patients in the HER2-low/HR-positive and triple-negative groups received 1.2 mg/kg of IV trastuzumab duocarmazine every 3 weeks. Seventeen patients in the HER2-positive group started with the same 1.2 mg/kg dose and then received 0.9 mg/kg every 3 weeks from cycle 5 onward. The remaining 16 HER2-positive patients started with 1.2 mg/kg every 3 weeks and then shifted to 1.2 mg/kg every 6 weeks from cycle 5 onward.
Patients across the study continued treatment until progression or unacceptable toxicity. Investigators performed tumor evaluation scans every 6 weeks. To manage toxicity, physicians could order dose reductions or delays of up to 42 days from the previous dose.
All patients were prescribed lubricating eye drops. Patients in the HER2-low/HR-positive and triple-negative arms also received prophylactic vasoconstrictive and anti-inflammatory eye drops 1 hour before infusion. Triple-negative patients continued using the drops 3 times per day for 48 hours.
Adverse events were reported for all 146 patients with various tumor types enrolled on the study. Thirty-four percent of patients required at least 1 dose delay and 16% needed dose reductions. Twenty-eight (19%) patients discontinued due to treatment-related adverse events (TRAEs), most often eye disorders.
There were no grade 4/5 treatment-related adverse events (TRAEs). The most common grade 3 TRAEs included neutropenia (6%), fatigue (3%), and conjunctivitis (3%). Investigators are still examining the impact of prophylactic eye drops on ocular toxicity.
The FDA granted trastuzumab duocarmazine a fast track designation in January 2018 as a potential treatment for patients with HER2-positive metastatic breast cancer that progressed during or after treatment with ≥2 HER2-targeting regimens for locally advanced or metastatic disease, or that progressed during or after treatment with T-DM1. The designation expedites the development and review of this antibody-drug conjugate in this setting.
Investigation into trastuzumab duocarmazine is ongoing in the multicenter, open-label, randomized phase III TULIP trial (NCT03262935). The primary objective is superiority for PFS at up to 2 years from baseline compared with physician’s choice of therapy in previously treated patients with HER2-positive unresectable locally advanced or metastatic breast cancer. Investigators are currently recruiting patients in the United States, Denmark, France, Italy, and the United Kingdom, with a targeted enrollment of 345.
Saura C, Thistlethwaite F, Banerji U, et al. A phase I expansion cohorts study of SYD985 in heavily pretreated patients with HER2-positive or HER2-low metastatic breast cancer. J Clin Oncol. 36, 2018 (suppl; abstr 1014).



