Medicine Is in His DNA: Giant in Breast Gene Research Draws on Childhood Values
Plenty of children are afraid to go to the doctor. Dennis Slamon used to look forward to it.
A Conversation With Dennis Slamon, MD, PhD
Plenty of children are afraid to go to the doctor. Dennis Slamon used to look forward to it.
“A career in medicine was what I wanted since I was 5 or 6, simply because of the remarkable doctor who took care of our family,” said Slamon, remembering the pediatrician who made house calls to treat him for a cold or flu. “He was very caring, very gentle, and very effective. I thought it would be great to be able to help people like that and make a family feel so good.”
Slamon, 62, the son of a coal worker and a homemaker, not only went on to become a physician, but also has realized his dream of helping people—hundreds of thousands of people, in fact. That’s how many patients have been treated with Herceptin (trastuzumab), the first molecularly targeted therapy for breast cancer.
During nearly 40 years spent researching and caring for patients, Slamon, now director of Clinical/ Translational Research at the Jonsson Comprehensive Cancer Center at the University of California, Los Angeles (UCLA), conducted the lab work and testing that resulted in Herceptin.
And when it comes to bedside manner, Slamon has lived up to his ideal, said Barbara Bradfield, the first patient to take Herceptin in phase I trials 19 years ago.
When Bradfield initially declined to take part in the trial, she said, Slamon called and begged her to reconsider.
“He worried all night, and he called me the next morning and asked me to go talk with him,” said Bradfield, who has had 12 tumors but has remained cancer-free since completing the trial. “When we met in person, he was so convincing. He’s got these beautiful, brown, soulful eyes, and he spent an hour and a half going through slides explaining everything, so I ended up saying yes—thank goodness.”
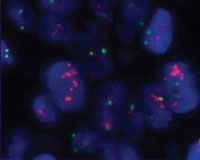
The orange staining shows HER2-positive tumor cells. Courtesy F. Hoffmann-La Roche Ltd.
Long Battle, Long Hours on Path to Herceptin
Approved by the FDA in 1998 and manufactured by Genentech, now part of the Roche Group, Herceptin is a monoclonal antibody that helps counteract a mutation of the HER2 gene, found in about 25% of breast cancer patients.
The intravenous drug, given in combination with or following chemotherapy, reduces recurrence rates by half in specific types of early HER2-positive breast cancer and by one-third in metastatic HER2- positive breast cancer, Slamon said. It increases survival by about 35% and 30% in those early and metastatic HER2-positive breast cancers, respectively, the researcher said.
The drug, which doesn’t cause such adverse events as the hair loss and nausea that often accompany conventional therapies, was also approved by the FDA last year for use in HER2-positive metastatic stomach cancer, in combination with chemotherapy.
Slamon fought for 12 years to get Herceptin to patients, keeping the project alive despite a nearly crippling early lack of funding, and ultimately helping to spark an understanding that breast cancer and other cancer types can take a variety of forms, each subtype potentially requiring its own treatment options. It is a principle that will prove true in all other major malignancies, Slamon believes, as the recent rise in targeted cancer therapies picks up speed during the next 5 years.
“We followed the data, and if it’s there and it says your approach is right, it doesn’t matter what anyone else’s preconceived notion is,” said Slamon, who has won nearly 2 dozen national research awards for his work during the last decade. “We never gave up when people said we were wasting our time.”
“We followed the data, and if it’s there and it says your approach is right, it doesn’t matter what anyone else’s preconceived notion is. We never gave up when people said we were wasting our time.”
Slamon is continuing his fight against cancer through his roles at UCLA, where he spends nearly half his time reviewing data and considering where it might lead.
“The highlight of my day is to meet with mid- and junior-level investigators and see this new stuff,” he said. “With colleagues capable of pushing the agenda in a positive way, we can think about exciting ideas.”
Serving as chief of UCLA’s Division of Hematology-Oncology and also a professor of Medicine, Slamon devotes about 30% of his hours to administrative duties, including raising money for research, another 20% to seeing cancer patients, and the remainder to teaching and giving lectures offsite.
As part of that work, he is helping to oversee clinical trials for new drug combinations that include Herceptin, as well as trials in collaboration with GlaxoSmithKline for a new HER2-blocking agent, Tykerb. In the lab, Slamon and his researchers are looking for new targeted treatments for ovarian, lung, and pancreatic cancers.
It’s a busy existence, one that has always required patience on the part of Slamon’s wife and 2 children, but the doctor is doing what he loves—and his patients can feel it. Nearly 2 decades after Slamon treated her, Bradfield thinks of the doctor every day and has his photo posted on her refrigerator.
“He’s been so caring, so dedicated, and so giving of his life,” Bradfield said. “We wish there were more of him.”

Dennis Slamon At a Glance
- Is 62 years old
- Is married and the father of 2 children: a 28-year-old daughter working for a film production company, and a 24-year-old son working in marketing and communications for Major League Baseball
- Enjoys fly fishing
- Was appointed by President Bill Clinton in 2000 to the 3-member President’s Cancer Panel
- Serves as director of the medical advisory board for the National Colorectal Cancer Research Alliance, a fundraising organization
- Is the subject of a Lifetime movie, Living Proof, and a book by Robert Bazell, HER-2: The Making of Herceptin, a Revolutionary Treatment for Breast Cancer
- Adheres to a simple research philosophy: “Follow the data.”
- Claims The Grapes of Wrath, by John Steinbeck, as his favorite book because “It tells the story of a time when people had to stick to the fundamentals they believed in to survive.”
- Likes the movie High Noon because the character of the marshal, without the support of his town, “had to stand against the gang.”
- Recalls doing heavy labor in a steel mill as his worst job ever. “It was repetitive and dirty,” he said. “I needed the money for school, so I did it.”
Mentors Spurred Interest in Oncology
Slamon ended up crossing paths with Bradfield and the larger oncology community, in part, because of a student teacher at his high school in New Castle, Pennsylvania. The teacher infused his lessons about biology with such enthusiasm that Slamon moved on to Washington & Jefferson College, in his home state, excited to learn more.
“I took all but one of the biology courses the school had to offer, because I couldn’t fit any more into my schedule,” he said. “I loved the topic, the diversity of it, and the more I learned, the more I thought about combining my interests in biology and medicine.”
Slamon did exactly that, simultaneously earning his medical degree and doctorate in cell biology in 1975 through a combined MD/PhD program at the Pritzker School of Medicine at the University of Chicago.
It was there that he began the research that paved the way for Herceptin. In the lab of Winston A. Anderson, PhD, a cell biologist in the Anatomy Department, and under the tutelage of Werner Kirsten, MD, of the Pathology Department, Slamon participated in research on retroviruses that caused cancer in mice.
“They were incredibly potent, more than anything we’d seen—acutely transformative retroviruses that caused cancer 2 to 3 weeks after injection,” Slamon said. “We learned, ultimately, that they were carrying an oncogene,” a gene with cancer-causing potential.


The actor Harry Connick Jr portrayed Slamon in the film, Living Proof, which depicts the researcher’s efforts to obtain funding for his cutting-edge science.
Exploring Proto-Oncogenes
That work led to a breakthrough several years later as Slamon completed a fellowship at UCLA’s Division of Hematology-Oncology.
“We realized that what these acutely transformed viruses were carrying that made them so potent was genes stolen from normal cells,” Slamon said. Once stolen, the researcher found, those genes—known as proto-oncogenes—were altered, becoming abnormal and contributing to the growth of cancer.
Slamon built on that knowledge in 1986, when he was asked by a Genentech researcher to look for siblings to the epidermal growth factor receptor, also known as HER1, a protein that sits on the surface of a cell and can cause cancer if mutated. One of the 6 genes Slamon was asked to investigate was HER2, and the results intrigued him.
“In 25% of breast tumors, we saw an alteration of gene amplification, an overabundance of numbers of the HER2 gene,” Slamon recalled. “Then, we realized that women whose tumors contained the alteration had a much different outcome. They had a more aggressive tumor that recurred more rapidly, and they died more quickly.”
The chilling finding proved something that would help change the face of cancer treatment.
“It told us right away that we were not dealing with 1 disease in breast cancer,” Slamon said, “even though the dogma at the time was that each disease was a monolith, defined by the tissue where it arose and treated with a one-size-fits-all approach.”
To Slamon, HER2 looked like a perfect target for treatment with an antibody, but not everyone agreed.
“No one was interested in pursuing antibodies because so many had failed,” Slamon said. “I was trying to convince Genentech to stay with the program based on the data, and it took a couple of years of hard sell. The company wasn’t terribly enthused, but there was a core of people there who believed in the data and kept the project alive.”
3 Questions for Dr Slamon
Is Herceptin being investiga ted for any new indications?
With Genentech, we’re investigating Herceptin in combination with another antibody, pertuzumab, for an improved rate of tumor disappearance in early HER2-positive breast cancer.
Genentech is also studying T-DM1 in early HER2-positive breast cancer. This combination attaches Herceptin and the chemotherapy DM1 together using a stable linker, designed to keep T-DM1 in 1 piece until it reaches specific cancer cells.
In collaboration with GlaxoSmithKline, we’re studying the combination of Herceptin with another HER2-blocking agent, Tykerb, to increase the antitumor effect in HER2-positive breast cancer.
Are you helping to conduct any other clinical trials?
With GlaxoSmithKline, we’re investigating whether Tykerb, added to chemotherapy, will help patients who have HER2-positive gastric cancer.
In addition, we have a trial going in ovarian cancer in collaboration with Amgen. The trial is testing another antibody to a different pathway we found that may play a role in a subtype of ovarian cancer that is very aggressive.
In the early stages of your efforts to create Herceptin, you had a hard time garnering support for your efforts. Do you still encounter that problem as you come up with new ideas?
It’s become a lot easier. We’ve proven the principle that this approach works if you have a drug targeting the right things.
Lining Up Private Funding
Luckily for Slamon, there were also private funders who felt certain he was on the right track.
One was Lilly Tartikoff (now Lilly Tartikoff Karatz), whose husband, Brandon, then president of NBC’s Entertainment Division, had been treated for cancer by Slamon. The other was Ronald O. Perelman, chairman of Revlon, a friend whom Tartikoff asked for support.
Initially, Slamon recalled, Perelman donated $1.8 million to help with his research. Several years later, in 1995, a spokeswoman said, Perelman gave $7.5 million to establish the Revlon/ UCLA Women’s Cancer Research Program, which Slamon still directs.
Millions more have been raised for Slamon’s research, first through an annual Fire and Ice Ball founded by Tartikoff and Perelman, and now through the yearly Revlon Run/Walk. And last year, the spokeswoman said, Revlon committed another $3 million dollars for use in Slamon’s translational labs and the Revlon/ UCLA Breast Center.
“Lilly told me what amazing work Denny was doing, and said that if he only had the funding, he could help many people,” recalled Perelman, who also is CEO and chairman of MacAndrews & Forbes Holdings. “After meeting Dr Slamon and seeing the potential in what he was working on, I immediately wanted to get involved. Denny is one of the most brilliant and dedicated researchers in medicine today, and his work has saved many women’s lives. I am so proud to have been able to help him accomplish that.”
With funding still difficult to come by for many scientists, Slamon wants to see every grant and donation used as effectively as possible. That’s why the researcher is involved with Stand Up To Cancer, a project of the Entertainment Industry Foundation that utilizes the star power of celebrities to raise funds aimed at slowing the competition between labs and bringing them together to collaborate.
“The idea that one lab will make progress quickly is archaic,” he said. “Putting funds behind the effort to bring labs together is a good experiment. We’ll see how it works.”
In the meantime, Slamon will continue to concentrate on the work that was his childhood dream—and the embodiment of the values he absorbed during those years.
“My parents taught us that doing something productive that could help others was the pinnacle of what you might want to achieve,” he recalled.
Patients like Bradfield know firsthand how thoroughly Slamon has accomplished that, and their well being makes the doctor proud.
His journey with Herceptin from the lab, through the clinic, and into the lives of patients has been “enormously gratifying,” Slamon said. “It’s what it’s all about.”
Beth Fand Incollingo is a NJ-based writer and editor, and owner of the communications firm Texterity, LLC.




