Charting the Course for Patients With High-Risk Colon Cancer: 3 Months Versus 6 Months
In 5 years, it is estimated that approximately 20% of patients with stage II disease and 35% with stage III disease will experience disease recurrence. These estimates highlight the need to pursue progress in adjuvant systemic therapy in order to decrease recurrence rates and improve survival.
Alexandre A. Jácome, MD, PHD

Colorectal cancer (CRC) is the second most common cause of cancer-related death in the United States.1 Despite recent improvements in screening rates, most patients with colon cancer (CC) receive a diagnosis of locally advanced disease (T3/T4 and/or node-positive) at first presentation.1 In 5 years, it is estimated that approximately 20% of patients with stage II disease and 35% with stage III disease will experience disease recurrence.2-4 These estimates highlight the need to pursue progress in adjuvant systemic therapy in order to decrease recurrence rates and improve survival.
Fluoropyrimidine-based adjuvant chemotherapy has been the standard of care of stage III CC for the past 30 years.2,4 However, the routine use of adjuvant chemotherapy in stage II CC has not been recommended, since the small improvements in disease-free survival (DFS) and in overall survival (OS) do not outweigh the expected rate of acute and late fluorouracil (5-FU)–related adverse events (AEs).5 Nevertheless, patients with stage II CC include a heterogeneous group who present with different risks of recurrence. The selection of patients with stage II disease who presumably derive larger benefit from adjuvant chemotherapy is based on the presence of prognostic clinicopathologic factors, which offer an inaccurate risk stratification in low- and high-risk stage II CC. There is no consensus regarding the clinicopathologic factors that should be considered in risk stratification. The National Comprehensive Cancer Network (NCCN) guidelines do consider the use of adjuvant 5-FU in patients with stage II CC who have fewer than 12 lymph nodes analyzed in the surgical specimen; poorly differentiated histology; lymphatic/vascular invasion; bowel obstruction; perineural invasion; localized perforation; and close, indeterminate, or positive margins.6 Likewise, the European Society for Medical Oncology guidelines take into account the presence of T4 or high preoperative carcinoembryonic antigen levels, in addition to the NCCN criteria.7
Cathy Eng, MD

The only predictive biomarker used in the selection of this patient population is the high-frequency microsatellite instability (MSI-H) status, expected to be found in approximately 15% of the stage II population. Patients with MSI-H tumors present a lower risk of recurrence and do not derive benefit from adjuvant chemotherapy with 5-FU alone, even if they are classified as high risk based on the aforementioned clinicopathologic factors.8,9 The identification of prognostic and predictive factors for a more accurate selection of patients with stage II CC who will benefit from adjuvant chemotherapy is urgently needed.
Stage III: Oxaloplatin-Based Adjuvant Chemotherapy for 3 Months or 6 Months?
Data from MOSAIC (NCT00275210) have established folinic acid (leucovorin), 5-FU, and oxaliplatin (FOLFOX) as the standard adjuvant therapy for stage III CC.10 Six-year follow-up data demonstrated that 6 months of FOLFOX was associated with a 7.5% absolute reduction in the risk of recurrence and 4.2% reduction in the risk of death in patients with stage III disease.4 Further studies confirmed the benefit of oxaliplatin- based adjuvant chemotherapy, including if used with either capecitabine (CAPOX) or bolus 5-FU (FLOX), with similar efficacy but with different toxicity profiles compared with infusional 5-FU.11,12 Therefore, apart from elderly patients, who might be considered to receive fluoropyrimidine alone because they derive a lower benefit from the addition of oxaliplatin,13 6-month oxaliplatin-based adjuvant chemotherapy should be offered to all patients with node-positive disease, irrespective of their T stage.
Nevertheless, 6-month oxaliplatin may be associated with several cumulative AEs, such as fatigue; liver injury; hypersplenism; and, mainly, peripheral neuropathy.14 Despite presenting a gradual resolution, approximately 15% of patients will experience grade 1 or higher neurotoxicity for over 4 years.4 To decrease the burdensome effects of oxaliplatin with a minimal loss of survival benefit, a noninferiority study (IDEA collaboration) was designed with the goal of prospectively pooling data from 6 randomized clinical trials of adjuvant therapy in patients with stage III CC to evaluate the hypothesis that 3 months of oxaliplatin-based therapy (FOLFOX or CAPOX) would be noninferior to 6 months in 3-year disease-free survival (DFS).15
IDEA collaboration was composed of 6 phase 3 clinical trials: CALGB/SWOG 80702, IDEA France, SCOT, ACHIEVE, TOSCA, and HORG (TABLE 116-21). In total, they evaluated 12,834 patients, of which approximately 60% were treated with FOLFOX and 40% with CAPOX. At a median follow-up of 41.8 months, noninferiority of 3 months of therapy versus 6 months was not confirmed in the modified intention-to-treat population.15 The 3-year DFS, the primary end point, in the 3-month group was 74.6% versus 75.5% in the 6-month group (HR, 1.07; 95% CI, 1.00-1.15; P = .11 for noninferiority of 3-month therapy; P = .045 for superiority of 6-month therapy). Noninferiority of 3 months versus 6 months could be claimed if the upper limit of the 2-sided 95% CI of the HR did not exceed 1.12.
TABLE 1. IDEA Collaboration Trials With Respective Characteristics and Efficacy Results16-21
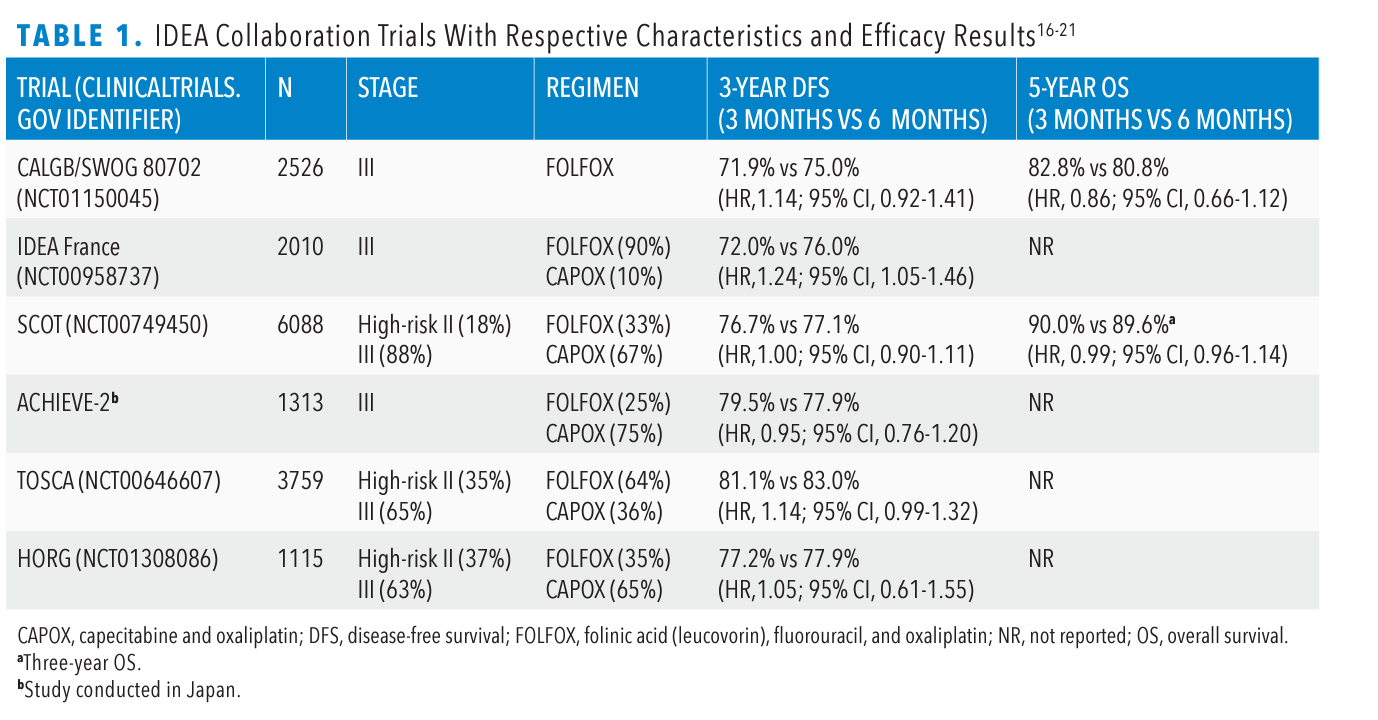
Updated data presented at the 2020 American Society of Clinical Oncology Virtual Scientific Program showed a 5-year OS of 82.4% versus 82.8%, respectively (HR, 1.02; 95% CI, 0.95-1.11; P = .0583 > 0.025 to reject the null hypothesis).22 In the 3-month group, grade 2 or higher neurotoxicity occurred in 16.6% and 14.2% of patients in the FOLFOX and CAPOX subgroups, respectively, compared with 47.7% and 44.9% in the 6-month group (P < .001).15 In addition, the shorter duration of oxaliplatin was associated with significantly lower rates of diarrhea, neutropenia, thrombocytopenia, nausea, mucositis, fatigue, and hand-foot syndrome.
Interestingly, a differential efficacy according to chemotherapy regimen was observed. Among the patients treated with FOLFOX, 6-month therapy was superior to 3-month in 3-year DFS (HR, 1.16; 95% CI, 1.07-1.26; P = .001 for superiority of 6-month therapy).22 On the other hand, the shorter duration of adjuvant therapy was noninferior to the longer duration among the patients who received CAPOX (HR, 0.98; 95% CI, 0.88-1.08). The interaction test was significant in the updated analysis (P = .0113).22
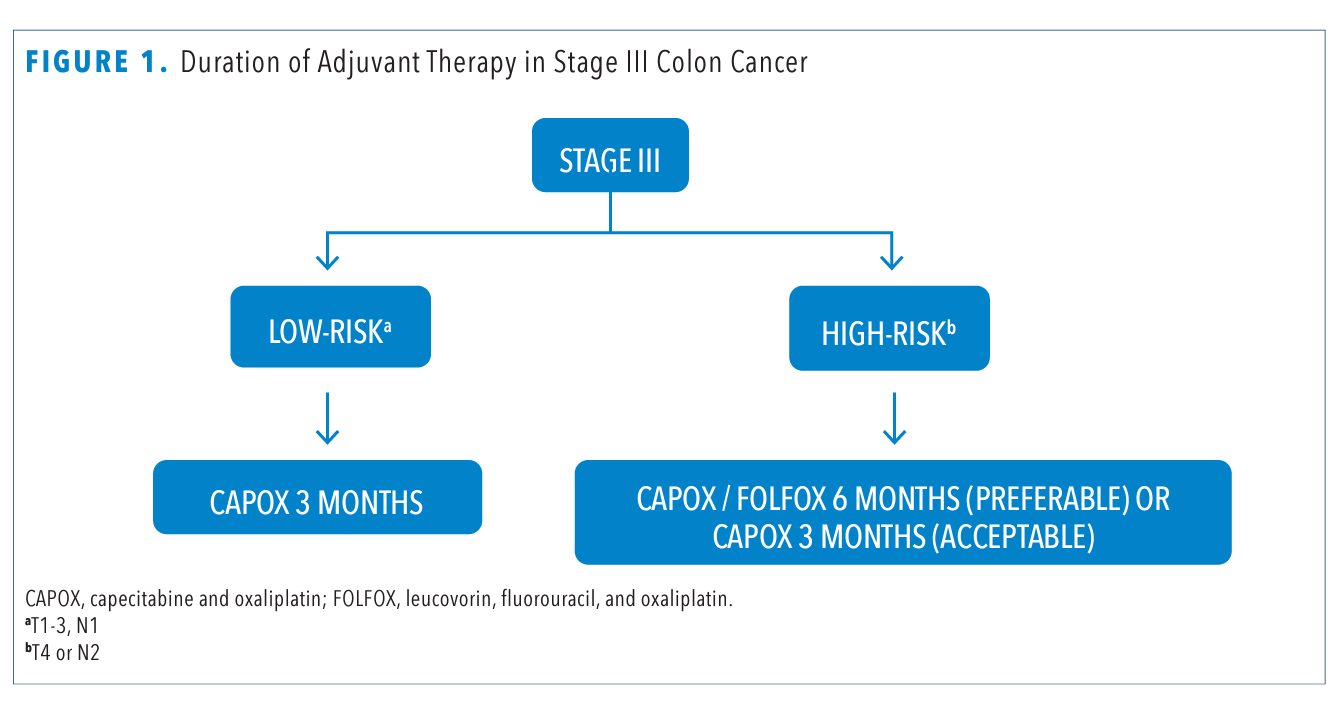
Subgroup analysis based on T and N stage also revealed a differential benefit of treatment duration. In patients deemed low risk with T1-3, N1 disease, 3-month therapy was noninferior to 6-month in 3-year DFS (HR, 1.01; 95% CI, 0.90-1.12).15 However, among the patients with high-risk cancers, T4 or N2, 6 months of therapy was superior to 3 months (HR, 1.12; 95% CI, 1.03-1.23; P = .01 for superiority). The interaction test between therapy duration and risk group was not significant (P = .11), how-ever. When treatment duration was analyzed according to risk stratification and chemotherapy regimen, 3 months of CAPOX was noninferior to 6 months in the low-risk group (HR, 0.85; 95% CI, 0.71-1.01). Further, 3 months of CAPOX compared well with 6 months even among the high-risk group (HR, 1.02; 95% CI, 0.89-1.17). But, independent of risk group, outcomes after 3 months of FOLFOX therapy were worse than those after 6 months.
The recently published post hoc analysis of the phase 3 IDEA France study (NCT00958737) showed the prognostic impact of tumor deposits in the DFS of patients with stage III CC.23 Tumor deposits were detected in 9.5% of patients (n = 181), who also presented with worse 3-year DFS: 65.6% versus 74.7% in patients with no tumor deposits (P = .007). Even in multivariable analysis adjusted for duration of adjuvant therapy, tumor deposits remained a strong prognostic factor (HR, 1.4; 95% CI, 1.1-1.8; P = .020). Interestingly, when the number of tumor deposits was added to the number of positive lymph nodes, 2.4% of the patients initially staged as pN1 were restaged as pN2. These restaged patients presented lower 3-year DFS compared with the pN1 population (60.7% vs 79.3%, respectively; P = .015), with similar 3-year DFS to those patients initially staged as pN2. This study sheds lights on the potential influence of the number of tumor deposits on the decision about the duration of adjuvant therapy (FIGURE 1).
In the 8th edition of AJCC: Cancer Staging Manual, patients with no regional lymph node metastases but with tumor deposits are staged as pN1c. However, the number of tumor deposits is not considered in the TNM staging system. The post hoc analysis of IDEA France suggests that pN1 patients who are restaged as pN2 based on the number of tumor deposits should be managed as high-risk stage III patients.
FIGURE 1. Duration of Adjuvant Therapy in Stage III Colon Cancer
High-Risk Stage II: 5-FU Alone or Oxalaplatin-Based Adjuvant Chemotherapy?
The routine use of any modality of adjuvant chemotherapy in patients with stage II CC has not been recommended. However, some of these patients present a similar or even higher risk of recurrence compared with stage III CC. Investigators enrolled 899 patients with stage II CC to the MOSAIC trial, and these patients did not derive statistically significant benefit from the addition of oxaliplatin, both in DFS and OS, even in the exploratory analysis of the high-risk population, defined as patients who presented at least 1 of the following: T4, tumor perforation, bowel obstruction, poorly differentiated tumor, venous invasion, or fewer than 10 lymph nodes examined.10
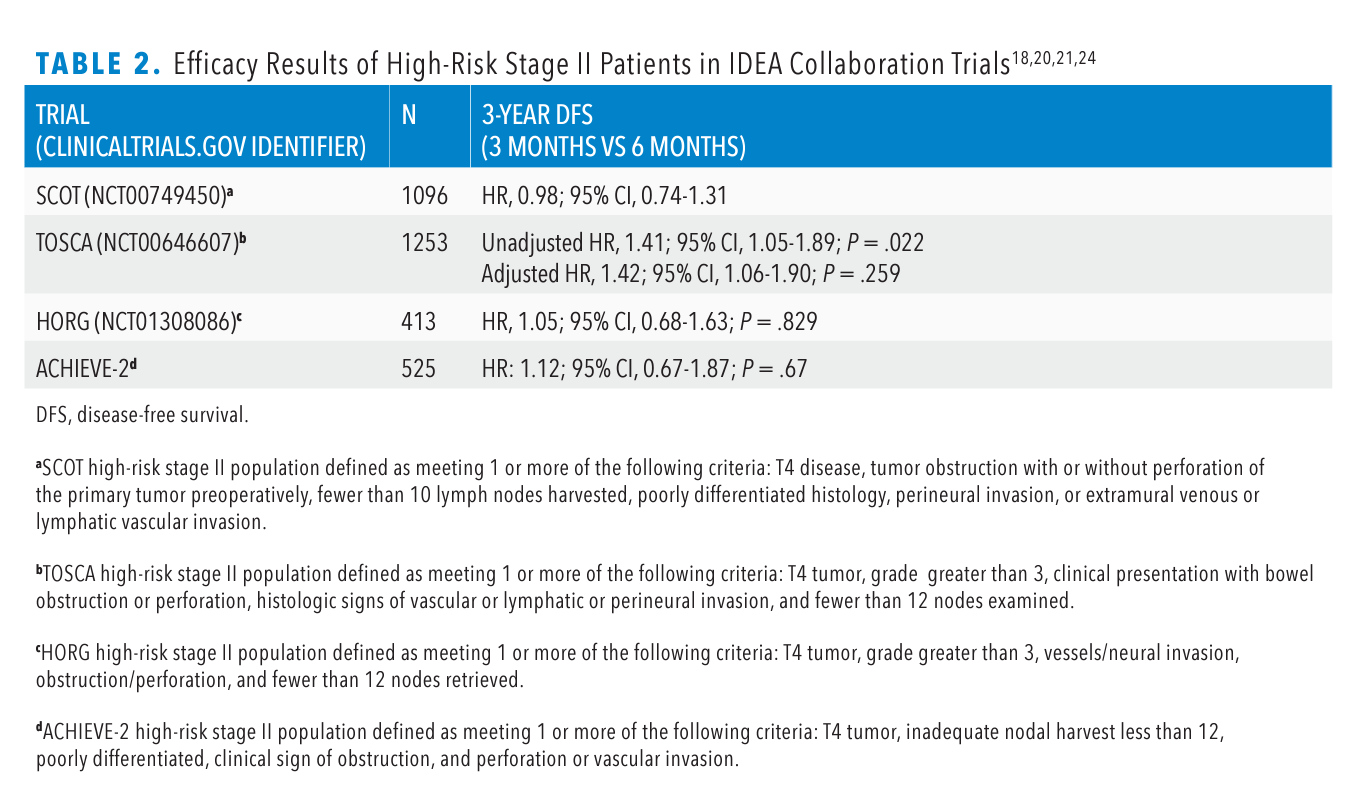
Additionally, 4 of the 6 clinical trials that composed IDEA collaboration included patients with stage II CC (TABLE 218,20,21,24). In total, 3273 patients with high-risk stage II CC were enrolled, despite having no consensus on the definition criteria of high-risk disease, which varied slightly among the 4 studies.
FOLFOX and CAPOX regimens were used in 1254 and 2019 patients, respectively. In a pooled analysis of the 4 trials, noninferiority of 3 months of therapy could not be demonstrated. The 5-year DFS rate was 80.7% with the 3-month regimen versus 84.0% with the 6-month regimen (HR, 1.18; 80% CI, 1.05-1.31; P = .404).25 Based on the data from the pooled analysis, these patients should be treated with 6-month oxaliplatin-based adjuvant therapy. Nevertheless, it has never been demonstrated that oxaliplatin plus fluoropyrimidine is superior over fluoropyrimidine alone in this population. None of the included trials had a third comparator arm for fluoropyrimidine alone.
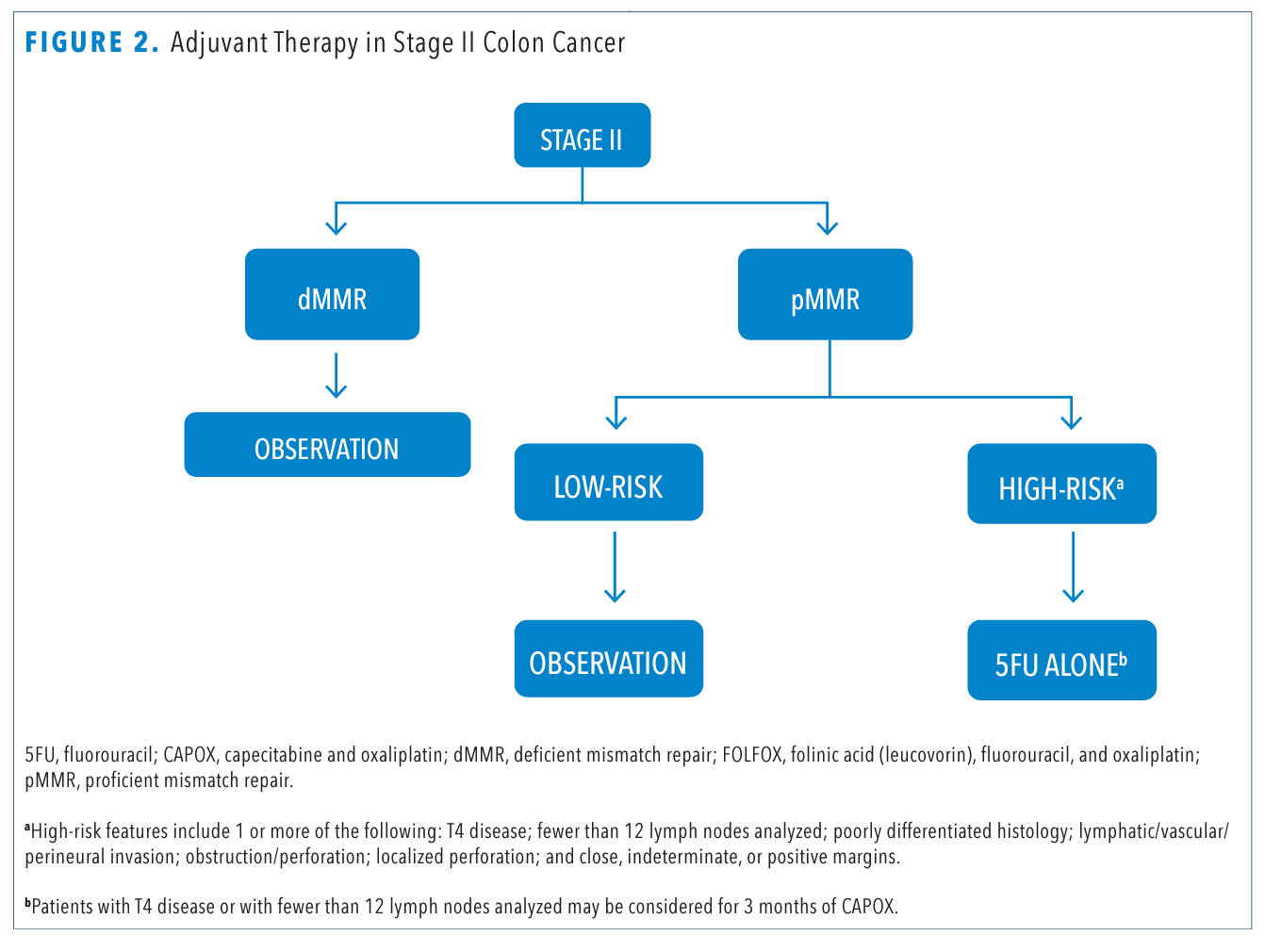
So, should a subgroup of stage II high-risk patients be treated with oxaliplatin-based adjuvant therapy? In the overall population of the IDEA collaboration, noninferiority of 3-month therapy could not be demonstrated in T4 patients (HR, 1.16; 95% CI, 1.03-1.31).15 Similarly, in a multivariate analysis of the Japanese ACHIEVE-2 trial, disease classified as T4 and involving fewer than 12 lymph nodes remained independent significant negative prognostic factors. Therefore, it is plausible to consider 3 months of oxaliplatin-based adjuvant therapy in patients who are staged T4, N0 or those with fewer than 12 lymph nodes harvested (FIGURE 2). Based on the overall findings from IDEA, it would be counterintuitive to offer 6 months of oxaliplatin- based adjuvant therapy in patients who are N0.
TABLE 2. Efficacy Results of High-Risk Stage II Patients in IDEA Collaboration Trials18,20,21,24
Perspectives
The decision to offer adjuvant therapy and its duration is regularly based on the TNM classification system, which provides useful yet incomplete prognostic information. Tumor infiltration by immune cells has been demonstrated to be valuable prognostic information. CD3+ and CD8+T cells in the tumor microenvironment may be measured and stratified by an Immunoscore, which separates the tumors into 3 categories: low (0%-25%), intermediate (25%-70%), and high (70%-100%).26
In data from a cohort of 1434 patients with stage II CC, Immunoscore was the highest relative contribution to the risk of recurrence of all clinical parameters, including the TNM classification system.26 Likewise, in a cohort of 763 patients with stage III CC, those with a high Immunoscore presented with the lowest risk of recurrence: 3-year recurrence-free rates were 56.9%, 65.9%, and 76.4% in patients with low, intermediate, and high Immunoscore, respectively (HR for high vs low, 0.48; 95% CI, 0.32-0.71; P = .0003).27 In multivariable analysis, Immunoscore was an independent prognostic variable for time to recurrence, even when adjusted for T stage, N stage, sidedness, and MSI status. Interestingly, adjuvant chemotherapy was significantly associated with survival in the high Immunoscore group for patients with both low-risk and high-risk stage III disease but not in the low-Immunoscore group.
Promising strategies to detect postoperative minimal residual disease through identification of circulating tumor DNA (ctDNA) have been described in CRC. In a cohort of 130 patients with stage I to III CRC, those who were ctDNA positive at postoperative day 30 were 7 times more likely to relapse than those who were ctDNA negative (HR, 7.2; 95% CI, 2.7-19.0; P < .001).28 Notably, those who were ctDNA positive following completion of adjuvant chemotherapy were 17 times more likely to relapse (HR, 17.5; 95% CI, 5.4-56.5; P < .001). In multivariate analyses, ctDNA status was independently associated with relapse after adjusting for known clinicopathologic risk factors. In addition, serial ctDNA analyses revealed disease recurrence up to 16.5 months ahead of standard radiologic imaging. COBRA (NCT04068103), a randomized phase 2/3 study, is under way to evaluate ctDNA as a predictive biomarker in adjuvant chemotherapy of patients with stage IIA CC.
Given the demonstrated benefit of immunotherapy in MSI-H metastatic CRC, an ongoing phase 3 study (NCT02912559) is evaluating the benefit of atezolizumab (Tecentriq) plus chemotherapy compared with chemotherapy alone in patients with stage III CC and MSI-H tumors. Furthermore, the optimistic results of genome-guided personalized therapy in metastatic disease, such as targeted therapy for patients who harbor BRAF V600E mutation, HER2 amplification, and NTRK fusion, provide hope that investigators will be able to address the potential benefit of targeted therapy in localized disease.
FIGURE 2. Adjuvant Therapy in Stage II Colon Cancer
Conclusions
Most patients with stage II and III CC are cured by surgery only. The identification of a subgroup of patients who need adjuvant chemotherapy thus far has been inaccurate. The decision to offer adjuvant chemotherapy based on the classical clinicopathologic factors induces a high risk of both overtreatment and undertreatment. The incorporation of prognostic and predictive biomarkers, such as Immunoscore and ctDNA, has the potential to bring precision medicine to the adjuvant therapy of CC.
The IDEA collaboration has brought vital elements to the shared decision-making process among patients and oncologists, who should consider the benefits of each regimen, its duration, and the treatment-related AEs, as well as the patient’s preferences, age, comorbidities, and expectations in the choice of adjuvant therapy.
In summary, it is acceptable to offer 3 months of CAPOX for patients with stage T1-3, N1 CC. Patients with T4 or N2 disease should be considered for 6-month oxaliplatin-based therapy, or 3 months of CAPOX if a minimal loss of benefit in DFS and OS is agreeable. Tumor deposits have demonstrated use as a robust prognostic factor, and their influence in determining the duration of adjuvant therapy should be carefully examined in further studies.
Although randomized clinical trials designed to specifically address the benefit of oxaliplatin in the adjuvant therapy of high-risk stage II CC hare not finished, the standard of care remains fluoropyrimidine alone. Patients with stage II CC who have fewer than 12 lymph nodes examined or with T4, N0 disease may be considered for 3 months of CAPOX.
References
- Siegel RL, Miller KD, Goding Sauer A, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70(3):145-164. doi:10.3322/caac.21601 2. Moertel CG, Fleming TR, Macdonald JS, et al. Levamisole and fluorouracil for adjuvant therapy of resected colon carcinoma. N Engl J Med. 1990;322(6):352-358. doi:10.1056/NEJM199002083220602
- Moertel CG, Fleming TR, Macdonald JS, et al. Levamisole and fluorouracil for adjuvant therapy of resected colon carcinoma. N Engl J Med. 1990;322(6):352-358. doi:10.1056/NEJM199002083220602
- Moertel CG. Accomplishments in surgical adjuvant therapy for large bowel cancer. Cancer. 1992;70(suppl 5):1364-1371. doi:10.1002/1097-0142(19920901)70:3+<1 364::aid-cncr2820701526>3.0.co;2-8
- Andre T, Boni C, Navarro M, et al. Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol. 2009;27(19):3109-3116. doi:10.1200/JCO.2008.20.6771
- Benson AB, 3rd, Schrag D, Somerfield MR, et al. American Society of Clinical Oncology recommendations on adjuvant chemotherapy for stage II colon cancer. J Clin Oncol. 2004;22(16):3408-3419. doi:10.1200/JCO.2004.05.063
- Benson AB, Venook AP, Al-Hawary MM, et al. NCCN guidelines insights: colon cancer, version 2.2018. J Natl Compr Canc Netw. 2018;16(4):359-369. doi:10.6004/ jnccn.2018.0021
- Argilés G, Tabernero J, Labianca R, et al. Localised colon cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020;31(10):12911305. doi:10.1016/j.annonc.2020.06.022
- Ribic CM, Sargent DJ, Moore MJ, et al. Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer. N Engl J Med. 2003;349(3):247-257. doi:10.1056/NEJMoa022289
- Sargent D, Marsoni S, Thibodeau S, et al. Confirmation of deficient mismatch repair (dMMR) as a predictive marker for lack of benefit from 5-FU based chemotherapy in stage II and III colon cancer (CC): a pooled molecular reanalysis of randomized chemotherapy trials. J Clin Oncol. 2008;26(suppl 15):4008. doi:10.1200/jco.2008.26.15_suppl.4008
- André T, Boni C, Mounedji-Boudiaf L, et al; Multicenter International Study of Oxaliplatin/5-Fluorouracil/Leucovorin in the Adjuvant Treatment of Colon Cancer (MOSAIC) Investigators. Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med. 2004;350(23):2343-2351. doi:10.1056/NEJMoa032709
- Schmoll H-J, Tabernero J, Maroun J, et al. Capecitabine plus oxaliplatin compared with fluorouracil/folinic acid as adjuvant therapy for stage III colon cancer: final results of the NO16968 randomized controlled phase III trial. J Clin Oncol. 2015;33(32):37333740. doi:10.1200/JCO.2015.60.9107
- Kuebler JP, Wieand HS, O’Connell MJ, et al. Oxaliplatin combined with weekly bolus fluorouracil and leucovorin as surgical adjuvant chemotherapy for stage II and III colon cancer: results from NSABP C-07. J Clin Oncol. 2007;25(16):2198-2204. doi:10.1200/JCO.2006.08.2974
- McCleary NJ, Meyerhardt JA, Green E, et al. Impact of age on the efficacy of newer adjuvant therapies in patients with stage II/III colon cancer: findings from the ACCENT database. J Clin Oncol. 2013;31(20):2600-2606. doi:10.1200/JCO.2013.49.6638.
- Overman MJ, Maru DM, Charnsangavej C, et al. Oxaliplatin-mediated increase in spleen size as a biomarker for the development of hepatic sinusoidal injury. J Clin Oncol. 2010;28(15):2549-2555. doi:10.1200/JCO.2009.27.5701
- Grothey A, Sobrero AF, Shields AF, et al. Duration of adjuvant chemotherapy for stage III colon cancer. N Engl J Med. 2018;378(13):1177-1188. doi:10.1056/NEJMoa1713709
- Meyerhardt JA, Shi Q, Fuchs CS, et al. Celecoxib in addition to standard adjuvant therapy with 5-fluorouracil, leucovorin, oxaliplatin (FOLFOX) in stage III colon cancer: results from CALGB/SWOG 80702. J Clin Oncol. 2020;38(suppl 15):4003. doi:10.1200/ JCO.2020.38.15_suppl.4003
- André T, Vernerey D, Mineur L, et al. Three versus 6 months of oxaliplatin-based adjuvant chemotherapy for patients with stage III colon cancer: disease-free survival results from a randomized, open-label, International Duration Evaluation of Adjuvant (IDEA) France, phase III trial. J Clin Oncol. 2018;36(15):1469-1477. doi:10.1200/ JCO.2017.76.0355
- Iveson TJ, Kerr RS, Saunders MP, et al. 3 versus 6 months of adjuvant oxaliplatin-fluoropyrimidine combination therapy for colorectal cancer (SCOT): an international, randomised, phase 3, non-inferiority trial. Lancet Oncol. 2018;19(4):562-578. doi:10.1016/S1470-2045(18)30093-7
- Yoshino T, Yamanaka T, Oki E, et al. Efficacy and long-term peripheral sensory neuropathy of 3 vs 6 months of oxaliplatin-based adjuvant chemotherapy for colon cancer: the ACHIEVE phase 3 randomized clinical trial. JAMA Oncol. 2019;5(11):1574-1581. doi:10.1001/jamaoncol.2019.2572
- Sobrero A, Lonardi S, Rosati G, et al. FOLFOX or CAPOX in stage II to III colon cancer: efficacy results of the Italian three or six colon adjuvant trial. J Clin Oncol. 2018;36(15):1478-1485. doi:10.1200/JCO.2017.76.2187
- Souglakos J, Boukovinas I, Kakolyris S, et al. Three-versus six-month adjuvant FOLFOX or CAPOX for high-risk stage II and stage III colon cancer patients: the efficacy results of Hellenic Oncology Research Group (HORG) participation to the International Duration Evaluation of Adjuvant Chemotherapy (IDEA) project. Ann Oncol. 2019;30(8):1304-1310. doi:10.1093/annonc/mdz19322.
- Sobrero AF, Andre T, Meyerhardt JA, et al. Overall survival (OS) and long-term disease-free survival (DFS) of three versus six months of adjuvant (adj) oxaliplatin and fluoropyrimidine-based therapy for patients (pts) with stage III colon cancer (CC): final results from the IDEA (International Duration Evaluation of Adj chemotherapy) collaboration. J Clin Oncol. 2020;37(suppl 15):4004. doi:10.1200/JCO.2020.38.15_suppl.4004
- Delattre JF, Cohen R, Henriques J, et al. Prognostic value of tumor deposits for disease-free survival in patients with stage III colon cancer: a post hoc analysis of the IDEA France phase III trial (PRODIGE-GERCOR). J Clin Oncol. 2020;38(15):1702-1710. doi: 10.1200/JCO.19.01960
- Manaka D, Shiozawa M, Kotaka M, et al. Impact of high-risk features on disease-free survival (DFS) in patients (pts) with high-risk stage II colon cancer (CC) in ACHIEVE-2 trial as part of the IDEA collaboration. J Clin Oncol. 2020;38(suppl 15):4011. doi:10.1200/ JCO.2020.38.15_suppl.4011
- Iveson T, Sobrero AF, Yoshino T, et al. Prospective pooled analysis of four randomized trials investigating duration of adjuvant (adj) oxaliplatin-based therapy (3 vs 6 months {m}) for patients (pts) with high-risk stage II colorectal cancer (CC). J Clin Oncol. 2019;37(suppl 15):3501. doi:10.1200/JCO.2019.37.15_suppl.3501
- Pagès F, Mlecnik B, Marliot F, et al. International validation of the consensus Immunoscore for the classification of colon cancer: a prognostic and accuracy study. Lancet. 2018;391(10135):2128-2139. doi:10.1016/S0140-6736(18)30789-X
- Mlecnik B, Bifulco C, Bindea G, et al. Multicenter International Society for Immunotherapy of Cancer study of the consensus immunoscore for the prediction of survival and response to chemotherapy in stage III colon cancer. J Clin Oncol. 2020;JCO1903205. doi:10.1200/JCO.19.03205
- Reinert T, Henriksen TV, Christensen E, et al. Analysis of plasma cell-free DNA by ultradeep sequencing in patients with stages I to III colorectal cancer. JAMA Oncol. 2019;5(8):1124-1131. doi:10.1001/jamaoncol.2019.0528