Immune-Stimulator Boosts Pembrolizumab in Melanoma Patients With "Cold" Tumors
Adding the immune stimulator ImmunoPulse IL-12 to pembrolizumab (Keytruda) produced promising activity among patients with melanoma identified as unlikely responders to anti–PD-1 therapies.
Adding the immune stimulator ImmunoPulse IL-12 to pembrolizumab (Keytruda) produced promising activity among patients with melanoma identified as unlikely responders to anti—PD-1 therapies.
Data from the phase II OMS-I102 trial presented at the 2017 World Congress of Melanoma showed that the combination induced an overall response rate (ORR) of 50% (n = 11) among 22 patients with baseline biomarker data suggesting they would not respond to anti—PD-1 therapy.
At 24 weeks’ follow-up, 41% (n = 9) of patients treated with the combination had a complete response (CR), 9% (n = 2) had a partial response (PR), and 9% had stable disease. The disease control rate was 59%.
Data were also presented at the meeting for 51 patients with melanoma enrolled in the phase II OMS-I100 study, which examined ImmunoPulse IL-12 monotherapy. The ORR in this study ranged from 25% to 34.6% for patients assigned to monotherapy. In 26 patients treated with ImmunoPulse IL-12 monotherapy on a 90-day cycle, 19.2% (n = 5) had CR, 15.4% (n = 4) had a PR, and 34.6% (n = 9) had stable disease. The disease control rate was 69.2%.
Twenty patients were treated with ImmunoPulse IL-12 on a 6-week cycle in a protocol addendum. Among these patients, there were no complete responders, but 25% of patients had a PR and 40% had stable disease. The disease control rate was 65%.
“We are encouraged by the data from these analyses, which continue to show that ImmunoPulse IL-12 can prime the immune system to help improve patient response to anti—PD-1,” Alain Algazi, MD, lead investigator and associate professor, department of Medicine (Hematology/Oncology), at the University of California San Francisco Helen Diller Family Comprehensive Cancer Center, said in a press release.
“The complete response rates observed in the phase II study assessing the combination of ImmunoPulse IL-12 and pembrolizumab in the predicted anti—PD-1 nonresponder patient population provide compelling early evidence that the combination could lead to a clinically meaningful impact on patient outcomes,” added Algazi.
Fewer than 10% of patients in both studies reported treatment related serious adverse events—9.8% of those assigned to monotherapy and 8.7% assigned to the combination.
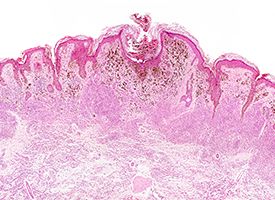
Highlighting their proprietary platform in a press release, OncoSec Medical explained, “IL-12 can trigger key immunologic events driving a cellular response leading to an inflamed tumor with increased TIL frequency whether as a monotherapy or combined with pembrolizumab, converting ‘cold’ tumors to ‘hot,’ which were further enhanced with the addition of an anti—PD1 antibody.”
In the release, Punit Dhillon, OncoSec president and CEO, said, “Collectively, these study findings reinforce the combination of ImmunoPulse IL-12 and pembrolizumab to address a significant unmet medical need in melanoma patients who are unlikely to respond to anti—PD-1 therapies.”
Dhillon added that the company will present additional data from the OMS-I102 combination trial at the upcoming 2017 Society for Immunotherapy of Cancer Annual Meeting. Additionally, initial data from PISCES/KEYNOTE-695 is scheduled to be released in mid-2018.
PISCES/KEYNOTE-695 is a global, multicenter phase IIb, open-label study of intratumoral plasma encoded IL-12 (tavokinogene telseplasmid) delivered by electroporation in combination with IV pembrolizumab in patients with stage III/IV melanoma who have progressed or are progressing on either pembrolizumab or nivolumab (Opdivo) treatment.
Algazi A, Tsai K, Bannavong D, et al. Clinical immune monitoring and biomarker data of pil-12 monotherapy compared to pil-12 with pembrolizumab in metastatic melanoma supports the rationale for combination therapy. Presented at: 9th World Congress of Melanoma; October 18-21, 2017; Brisbane, Australia. Abstract FC05-3.



