Publication
Article
Current and Emerging Treatments for Gastroenteropancreatic Neuroendocrine Tumors
Author(s):
During an OncLive® scientific interchange, panelists discussed the current treatment landscape for patients with gastroenteropancreatic-neuroendocrine tumors and the need for improved novel therapies.
Approximately 175,000 Americans are affected by neuroendocrine tumors (NETs), 65% of which are gastroenteropancreatic (GEP) NETs. GEP-NETs represent a diverse family of tumors that arise in the gastrointestinal (GI) tract or pancreas.1-3 The overall incidence of NETs across all stages, sites, and grades has increased nearly 7-fold over the past 40 years, a greater increase than that of all other malignant neoplasms; this may be partly credited to enhanced technologies for detecting early-stage disease and stage migration.1
The increasing incidence of GEP-NETs heightens the urgency to improve diagnostic and treatment approaches for these complex tumors. Regarding diagnostics, next-generation genetic sequencing techniques have gained traction, helping to identify patients at risk for future disease or in very early stages of disease. However, to guide individualized treatment decisions, additional research is needed to understand how specific genetic mutations influence GEP-NET behaviors.4,5 Evolving approaches are already helping investigators identify new biomarkers that may serve as better indicators for accurate GEP-NET diagnosis, prognosis, and therapy response than traditional biomarkers, which can sometimes lead to false positives (eg, chromogranin A, which increases in many non—GEP-NET conditions) or involve cumbersome testing (eg, insulin or gastrin).6 A large opportunity exists in research to identify biomarkers for poorly differentiated and high-grade tumors.
In terms of treatment options, most patients with GEP-NETs are not candidates for curative surgery, so they are offered long-term systemic treatment for antitumor effects and symptom relief.7 The current treatment landscape for GEP-NETs and the need for improved novel therapies was discussed on January 23, 2020, in San Francisco, California, during an OncLive® scientific interchange titled “Current and Emerging Treatments for Neuroendocrine Tumors.” The interchange was led by Carina Mari Aparici, MD, of Stanford University. Panelists were Walid Shaib, MD, of Emory University School of Medicine; Aman Chauhan, MD, of the University of Kentucky; Andrew E. Hendifar, MD, of Cedars-Sinai Medical Center in Los Angeles; Thomas Hope, MD, of the University of California, San Francisco; and Hagen F. Kennecke, MD, MHA, FRCPC, of Virginia Mason Medical Center. This article summarizes key data and discussion points from this scientific interchange, including current GEP-NET therapies—such as somatostatin analogues (SSAs), peptide receptor radionuclide therapy (PRRT), and emerging novel drugs—and their clinical trial data, as well as institutions’ varying therapy-sequencing strategies and the need for further research and guidelines for treating this complex disease.
Current Treatment Landscape
GEP-NET Grading System
The World Health Organization (WHO) 2010 and 2017 classification system categorizes GEP-NETs into 3 grades on the basis of histological differentiation and cell proliferation index, which assists in guiding treatment decisions. Tumor grade is determined by the highest number of either Ki-67 protein or mitotic count, and it offers an important prognostic value for GEP-NETs. Median survival rates have been determined for all NETs across all locations by tumor grade. For individuals with grade 1 tumors, median survival is more than 16 years; for grade 2, about 8 years; and for grade 3, about 10 months.8 In 2017, WHO updated the staging classifications for pancreatic NETs (pNETs) to recognize well-differentiated grade 3 tumors. This will allow for more precisely targeted treatment options for grade 3 tumors. Poorly differentiated grade 3 pNETs may continue to be treated with standard systemic chemotherapy, whereas well- and moderately differentiated grade 3 pNETs have been shown to benefit from targeted therapies (everolimus or sunitinib). Well-differentiated pNETs may even benefit from surgery.8
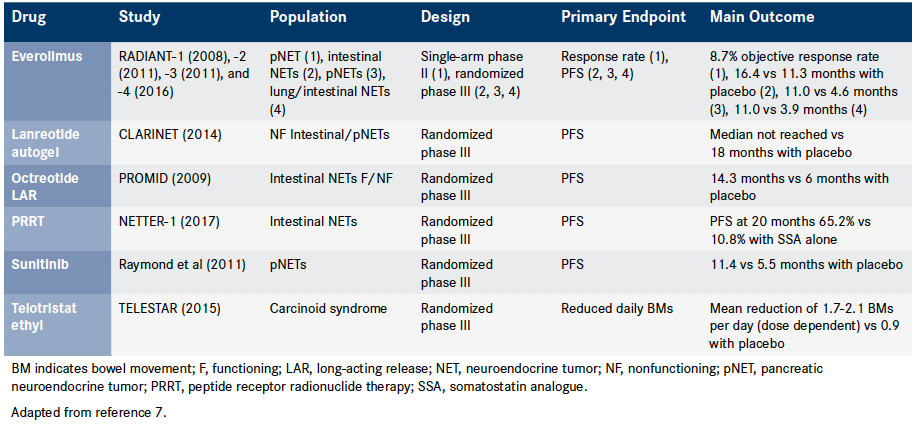
Surgery, the only curative treatment for GEP-NETs, is generally considered a first-line treatment for localized NETs.7 However, despite advances in diagnostics, GEP-NETs are often not identified for up to 5 to 7 years after clinical symptoms appear, as the symptoms are not specific. Approximately 21% of well-differentiated NETs, 30% of moderately differentiated NETs, and 50% of poorly differentiated or undifferentiated NETs are diagnosed in the metastatic stage.9 Thus, a substantial number of patients with GEP-NETs are not candidates for surgery and require systemic therapy after diagnosis (Table).7
Somatostatin Analogues
SSAs are generally considered first-line treatments for longterm systemic treatment of GEP-NETs.7 They are structured similarly to somatostatins, which are naturally occurring peptides that decrease the secretion of GI hormones, inhibit blood flow, and hinder cell proliferation. SSAs differ from somatostatins by providing a longer half-life,10 and they offer symptom control and antitumor effects for GEP-NETs. SSAs— specifically, octreotide and lanreotide—received a category 2A recommendation in 2019 from the National Comprehensive Cancer Network (NCCN) for managing GEP-NETs.11
In 1988, octreotide became the first SSA approved by the FDA. Octreotide long-acting release (LAR) is indicated for severe diarrhea and flushing episodes associated with metastatic carcinoid tumors. It is also indicated for long-term treatment of the profuse watery diarrhea associated with vasoactive intestinal peptide-secreting tumors in patients in whom initial treatment with immediate-release octreotide has been effective and tolerated.12,13 In PROMID, a phase IIIb, randomized, double-blind, placebo-controlled trial, octreotide LAR also demonstrated an antiproliferative effect in patients with metastasized NETs of the midgut (N = 85). The median time to tumor progression was 14.3 versus 6.0 months for the octreotide LAR and placebo groups, respectively (HR, 0.34; 95% CI, 0.20-0.59; P = .000072). After 6 months of treatment, 66.7% of patients receiving octreotide LAR and 37.2% receiving placebo experienced stable disease.14
Lanreotide, approved for adults by the FDA in 2007, is an SSA to slow the growth of GEP-NETs that have spread or cannot be removed by surgery. It is also indicated to treat carcinoid syndrome to reduce the need for the use of short-acting SSAs.15 The antitumor effects of lanreotide on GEP-NETs were demonstrated in CLARINET, a phase III, randomized, double-blind, placebo-controlled trial in 204 adult patients with metastatic grade 1 or 2 enteropancreatic NETs. Patients on lanreotide experienced significantly longer progression-free survival (PFS) than those on placebo (median not reached vs median of 18.0 months; HR, 0.47; 95% CI, 0.30-0.73; P <.001 by the stratified log-rank test), with a 53% reduction in risk of disease progression or death.16
In the real world, the decision to start patients on an SSA is often based on whether patients exhibit symptoms. Patients who are symptomatic, particularly if they have carcinoid syndrome, are typically started on an SSA to manage symptoms. For those who are asymptomatic, some clinicians prefer to monitor until progression to protect their patients from toxicities and to reduce the financial burden associated with SSAs, particularly because many patients may not progress for several years. Delaying therapy can also give clinicians the opportunity to more accurately identify the pace of disease progression. However, this approach can vary, and certain patients, such as those with a high-bulk disease, may warrant a more aggressive treatment with SSAs up front. If there is a concern regarding SSA tolerance, patients may be started on a week of a short-acting SSA to confirm absence of an allergic response before initiating a long-acting SSA.
Peptide Receptor Radionuclide Therapy
PRRT uses radiopharmaceuticals, such as 90Y-DOTA-Tyr3-octreotide and 177Lu-DOTA-Tyr3-octreotate (177Lu-Dotatate), that are developed by combining a synthetic SSA with a β-emitting radioisotope. These radiocompounds differ by their energetic features (because of the radionuclide) and peptide receptor affinity (because of the analogue) and bind to somatostatin receptors that are typically overexpressed in NETs.17 PRRT with 177Lu-Dotatate is indicated for the treatment of somatostatin receptor—positive GEP-NETs (including foregut, midgut, and hindgut); it is an NCCN category 1 recommendation for midgut tumors with somatostatin receptor–positive imaging and progression on octreotide or lanreotide.11,18 The NCCN recommends that patients with hormonally functioning tumors should continue octreotide or lanreotide treatment along with 177Lu-Dotatate. Because SSAs and 177Lu-Dotatate can compete for somatostatin receptor binding, patients should not receive long-acting SSAs for 4 to 6 weeks before each 177Lu-Dotatate treatment, nor should they receive short-acting SSAs within 24 hours before each 177Lu-Dotatate treatment. These patients may receive short- or long-acting SSAs 4 to 24 hours after each 177Lu-Dotatate treatment.11
177Lu-Dotatate in combination with an SSA has demonstrated efficacy for the treatment of GEP-NETs. NETTER-1, a phase III, randomized, placebo-controlled trial, evaluated the efficacy and safety of 177Lu-Dotatate plus octreotide supportive therapy in patients with advanced, progressive, somatostatin receptor—positive midgut NETs. At month 20, the estimated rate of PFS was 65.2% for the 177Lu-Dotatate group (95% CI, 50.0%-76.8%) and 10.8% for the control group receiving only octreotide LAR (95% CI, 3.5%-23.0%). 177Lu-Dotatate also demonstrated a significantly higher response rate than that of only octreotide LAR (18% vs 3%; P <.001).19 In PRELUDE, an international, retrospective, noncomparative analysis using patient medical records, the combination of 177Lu-Dotatate and lanreotide showed promise for treating patients with progressive NETs in the lung (n = 1) or digestive system (n = 39). Although enrollment ended prematurely because of insufficient recruitment, data for effectiveness were encouraging.20
Table. Clinical Trial Data for Gastroenteropancreatic Neuroendocrine Tumor Therapies7 (Click to Enlarge)
Mammalian Target of Rapamycin Inhibitors
The mTOR is a serine-threonine kinase that stimulates cell proliferation, growth, and angiogenesis. It is involved in the pathogenesis of NETs. Inhibiting mTOR has resulted in a substantial antiproliferative effect on pNETs.22 The mTOR inhibitor everolimus, an NCCN category 2A recommendation for NETs, is indicated for adults with progressive pNETs and adults with progressive, well-differentiated, nonfunctional NETs of GI or lung origin that are unresectable, locally advanced, or metastatic. Its safety and efficacy in treating patients with carcinoid syndrome have not yet been determined.11,23 In RADIANT-3 and RADIANT-4, which were phase III, randomized, double-blind, placebo-controlled trials, PFS was more than double for those in the everolimus groups compared with those in the placebo groups. In patients with pNETs (RADIANT-3; n = 410), everolimus reduced risk of progression or death by 65%, with a median PFS of 11.0 versus 4.6 months with placebo (HR, 0.35; 95% CI, 0.27-0.45; P <.001).22 For patients with GI and lung NETs (RADIANT 4; n = 302), everolimus reduced the estimated risk of progression or death by 52% (HR, 0.48; 95% CI, 0.35-0.67; P <.00001). The median PFS was 11.0 months with everolimus and 3.9 months with placebo.24
Everolimus is generally considered to be a third-line treatment for GEP-NETs after SSAs and PRRT, but the sequence can vary by disease characteristics. For patients with a pNET, the chemotherapy combination capecitabine—temozolomide (CAPTEM) may have a therapeutic opportunity equal to that of everolimus. Clinicians agree that everolimus should not be used either as a first-line option for high-burden disease (such as GEP-NETs with more than 80% liver involvement) or for a functional carcinoid accompanied by flushing and diarrhea. Everolimus may be appropriate as first-line treatment for patients with a low-volume small bowel NET or for those with insulinoma.
Multitarget Tyrosine Kinase Inhibitors
Eventually, resistance develops to the systemic therapies available for GEP-NETs, compromising PFS.25 At a cellular level, resistance can occur because of the congregation of many receptors on the same intracellular mechanisms, which allows an activated receptor system to bypass an inhibited system. Multitarget tyrosine kinase inhibitors (MTKIs), which compete with adenosine triphosphate to bind with cell surface receptors and ultimately block angiogenesis and tumor activity, have shown promise with mitigating this resistance by simultaneously targeting multiple receptors. Several MTKIs are currently being developed as novel therapies for solid tumors.26
In the TALENT trial, the MTKI lenvatinib demonstrated promising PFS and OS for pretreated patients with pNETs and GI NETs (N = 111). Patients were treated with lenvatinib until disease progression or intolerable toxicity. With a 19-month median follow-up, patients with pNETs experienced a 15.5-month PFS (95% CI, 11.3—not reached) and a 29.2-month OS (95% CI, 23.2–not reached). Those with GI NETs experienced a 15.4-month PFS (95% CI, 11.5-19.4) and OS was not reached. The overall response rate (ORR) was 42.0% for pNETs and 16.3% for GI NETs. According to the investigators, these results demonstrate the highest ORR by central radiology assessment to a targeted agent in this particular setting.25
The MTKI sunitinib is approved for the treatment of progressive, well-differentiated pNETs in patients with unresectable locally advanced or metastatic disease.27 Although data on sunitinib are limited, the therapy has demonstrated an increase in PFS for progressive, metastatic, welldifferentiated pNETs in phase III and phase IV clinical trials.28
Novel Therapies
A substantial need still exists for novel therapies in the treatment of GEP-NETs to improve efficacy and reduce radiation and toxic adverse effects. Once patients have exhausted appropriate treatment options, clinicians often encourage participation in clinical trials of new therapies. Multiple trials are currently being conducted to explore the therapeutic effects of immunotherapies for NETs; while data are currently limited, immunotherapies have demonstrated safety and efficacy in the treatment of other cancers.29,30 Immunotherapies are sometimes used in clinical practice for high-grade, poorly differentiated GEP-NETs. Well-differentiated, low-grade GEPNETs are not immunogenic, so clinicians hesitate to administer immunotherapy to this population.
Treatment combinations—including triplet combinations— are also being explored through preclinical and clinical trials. Initial results have been positive; however, large randomized trials are needed to generate strong evidence that supports their safety and efficacy. The primary limitations to combination therapies are sensitization and toxicity.
Sequencing Strategies and Personalized Medicine
The expanding targeted treatment options increase the need for national guidelines on therapy strategy and sequencing, which have not yet been established. The 2019 NCCN Guidelines state that no data currently support a specific sequence of regional versus systemic therapy or a sequence for systemic therapies.11 As stated previously, surgery is typically first-line treatment for localized tumors, and SSAs often serve as first-line options for systemic treatment.7 PRRT is often initiated once patients progress on an SSA,11 and mTOR inhibitors, chemotherapy (such as CAPTEM), MTKI, and novel therapies may be used as well to address symptoms and slow progression. Although many institutions have generated their own treatment guidelines for internal use, these approaches can vary considerably.
When selecting and sequencing therapies, clinicians must consider patient preferences, finances, and quality of life in addition to tumor grade, tumor burden, and timing of disease progression. Every patient presents with the disease differently, running the gamut from being asymptomatic to experiencing symptoms from the primary disease to having stage IV metastatic disease with liver symptomatology. Some tumors may be more hepatic than others, and some tumors are refractory to PRRT from the start. Each patient requires a unique treatment approach, and clinicians continue to grapple with identifying the optimal therapeutic regimen at the individual level, because of a lack of both treatment guidelines and data to help guide decision making. Because most clinical trials on therapies for GEP-NETs involve a heterogenous group of patients not separated by WHO classification for tumor grade (because of difficulties with proper stratification during trials), clinicians do not have data on the efficacy of a drug in patients with a specific tumor grade. It is difficult to predict how a grade 1 tumor versus a grade 2 tumor will respond to a therapy.
Conclusions
All available therapies for GEP-NETs, whether as monotherapy or in combination, are currently leveraged to treat this complex, diverse population of patients, yet no treatment has maintained PFS indefinitely. Clinicians acknowledge that many aspects of GEP-NETs are still unknown, and substantial efforts must be made to better understand the disease while advancing treatment options. There is a particular need for phase II and III clinical trials to gain insight into treatment for grade 3 tumors, which have received less attention in the past because of grade 3 tumor rarity and poor pathology.
Research efforts are pushing toward improvements in therapies; patients with GEP-NETs as well as clinicians who treat the disease are invested in understanding the disease and improving outcomes. Patients actively engage in online discussions, and many clinicians refer appropriate patients to participate in clinical trials for novel therapies that may advance safety and efficacy. The number of such trials is on the rise as the healthcare community recognizes opportunities to improve GEP-NET treatment. Investigators are also working to identify additional biomarkers for improved diagnosis, prognosis, and therapy response.6
Nonetheless, GEP-NETs currently remain difficult to treat, and it is not possible to apply a single set of treatment principles to all patients. Although building treatment sequencing guidelines for patients can be helpful, assessing the response in each patient is most important for determining the most promising course of therapy. The therapeutic approach also involves deciding when to re-treat (eg, choosing whether to administer CAPTEM for either 12 months consecutively or 6 months with a subsequent break before reinitiating therapy). Until GEP-NETs and therapeutic approaches are more fully understood, clinicians may find support in their quest to determine the right treatment courses for their patients by creating and participating in community forums with other oncologists to learn as much as possible about the various approaches and outcomes.
References
- Dasari A, Shen C, Halperin D, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017;3(10):1335-1342. doi: 10.1001/jamaoncol.2017.0589.
- Zuetenhorst JM, Taal BG. Metastatic carcinoid tumors: a clinical review. Oncologist. 2005;10(2):123-131. doi: 10.1634/theoncologist.10-2-123.
- Lawrence B, Gustafsson BI, Chan A, et al. The epidemiology of gastroenteropancreatic neuroendocrine tumors. Endocrinol Metab Clin North Am. 2011;40(1):1-18, vii. doi: 10.1016/j.ecl.2010.12.005.
- O’Shea T, Druce M. When should genetic testing be performed in patients with neuroendocrine tumours? Rev Endocr Metab Disord. 2017;18(4):499-515. doi: 10.1007/s11154-017-9430-3.
- Kawasaki K, Fujii M, Sato T. Gastroenteropancreatic neuroendocrine neoplasms: genes, therapies and models. Dis Model Mech. 2018;11(2):dmm029595. doi: 10.1242/dmm.029595.
- Sansone A, Lauretta R, Vottari S, et al. Specific and non-specific biomarkers in neuroendocrine gastroenteropancreatic tumors. Cancers (Basel). 2019;11(8):E1113. doi: 10.3390/cancers11081113.
- Uri I, Grozinsky-Glasberg S. Current treatment strategies for patients with advanced gastroenteropancreatic neuroendocrine tumors (GEP-NETs). Clin Diabetes Endocrinol. 2018;4:16. doi: 10.1186/s40842-018-0066-3.
- Deguelte S, de Mestier L, Hentic O, et al. Preoperative imaging and pathologic classification for pancreatic neuroendocrine tumors. J Visc Surg. 2018;155(2):117-125. doi: 10.1016/j.jviscsurg.2017.12.008.
- Vinik AI, Woltering EA, Warner RR, et al; North American Neuroendocrine Tumor Society (NANETS). NANETS consensus guidelines for the diagnosis of neuroendocrine tumor. Pancreas. 2010;39(6):713-734. doi: 10.1097/ MPA.0b013e3181ebaffd.
- de Herder WW, Hofland LJ, van der Lely AJ, Lamberts SW. Somatostatin receptors in gastroentero-pancreatic neuroendocrine tumours. Endocr Relat Cancer. 2003;10(4):451-458. doi: 10.1677/erc.0.0100451.
- National Comprehensive Cancer Network. Clinical Practice Guidelines in Oncology. Neuroendocrine and Adrenal Tumors (version 1.2019). nccn.org/ professionals/physician_gls/pdf/neuroendocrine.pdf. Published March 5, 2019. Accessed February 20, 2020.
- Sandostatin LAR Depot [prescribing information]. East Hanover, NJ: Novartis Pharmaceuticals Corp; 2019. www.pharma.us.novartis.com/sites/www.pharma. us.novartis.com/files/sandostatinlar.pdf. Accessed February 18, 2020.
- Wolin EM. The expanding role of somatostatin analogs in the management of neuroendocrine tumors. Gastrointest Cancer Res. 2012;5(5):161-168.
- Rinke A, Müller HH, Schade-Brittinger C, et al; PROMID Study Group. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID Study Group. J Clin Oncol. 2009;27(28):4656-4663. doi: 10.1200/JCO.2009.22.8510.
- Somatuline Depot [prescribing information]. Cambridge, MA: Ipsen Biopharmaceuticals Inc; 2019. ipsen.com/websites/Ipsen_Online/wp-content/ uploads/2019/08/30162316/Somatuline_Depot_Full_Prescribing_Information_ 7.22.19.pdf. Accessed February 18, 2020.
- Caplin ME, Pavel M, Ćwikła JB, et al; CLARINET Investigators. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med. 2014;371(3):224-233. doi: 10.1056/NEJMoa1316158.
- Severi S, Grassi I, Nicolini S, et al. Peptide receptor radionuclide therapy in the management of gastrointestinal neuroendocrine tumors: efficacy profile, safety, and quality of life. Onco Targets Ther. 2017;10:551-557. doi: 10.2147/ OTT.S97584.
- Lutathera [prescribing information]. Millburn, NJ: Advanced Accelerator Applications USA Inc; 2018. s3-eu-west-1.amazonaws.com/s3-lutathera/ wp-content/uploads/2018/07/12100815/LUTATHERA_lutetium_Lu_177_ dotatate_FDA_Prescribing_Information.pdf. Accessed February 25, 2020.
- Strosberg J, El-Haddad G, Wolin E, et al; NETTER-1 Trial Investigators. Phase 3 trial of 177Lu-dotatate for midgut neuroendocrine tumors. N Engl J Med. 2017;376(2):125-135. doi: 10.1056/NEJMoa1607427.
- Prasad V, Srirajaskanthan R, Toumpanakis C, et al. Lanreotide depot/autogel before, during, and after peptide receptor radionuclide therapy (PRRT) in advanced neuroendocrine tumors (NETs): data from the PRELUDE study. J Clin Oncol. 2018;36(15 suppl; abstr e16167). doi: 10.1200/JCO.2018.36.15_ suppl.e16167.
- Efficacy and safety of 177Lu-edotreotide PRRT in GEP-NET patients (COMPETE). clinicaltrials.gov/ct2/show/NCT03049189. Updated February 13, 2020. Accessed February 25, 2020.
- Yao JC, Shah MH, Ito T, et al; RAD001 in Advanced Neuroendocrine Tumors, Third Trial (RADIANT-3) Study Group. Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med. 2011;364(6):514-523. doi: 10.1056/ NEJMoa1009290.
- Afinitor [prescribing information]. East Hanover, NJ: Novartis Pharmaceuticals Corp; 2020. novartis.us/sites/www.novartis.us/files/afinitor.pdf. Accessed March 24, 2020.
- Yao JC, Fazio N, Singh S, et al; RAD001 in Advanced Neuroendocrine Tumours, Fourth Trial (RADIANT-4) Study Group. Everolimus for the treatment of advanced, non-functional neuroendocrine tumours of the lung or gastrointestinal tract (RADIANT-4): a randomised, placebo-controlled, phase 3 study. Lancet. 2016;387(10022):968-977. doi: 10.1016/S0140-6736(15)00817-X.
- Capdevila J, Fazio N, Lopez Lopez C, et al. Final results of the TALENT trial (GETNE1509): a prospective multicohort phase II study of lenvatinib in patients (pts) with G1/G2 advanced pancreatic (panNETs) and gastrointestinal (giNETs) neuroendocrine tumors (NETs). J Clin Oncol. 2019:37(15 suppl; abstr 4106). doi: 10.1200/JCO.2019.37.15_suppl.4106.
- Grillo F, Florio T, Ferraù F, et al; NIKE Group. Emerging multitarget tyrosine kinase inhibitors in the treatment of neuroendocrine neoplasms. Endocr Relat Cancer. 2018;25(9):R453-R466. doi: 10.1530/ERC-17-0531.
- Sutent [prescribing information]. New York, NY: Pfizer Inc; 2019. labeling. pfizer.com/showlabeling.aspx?id=607. Accessed March 24, 2020.
- Raymond E, Kulke MH, Qin S, et al. Efficacy and safety of sunitinib in patients with well-differentiated pancreatic neuroendocrine tumours. Neuroendocrinology. 2018;107(3):237-245. doi: 10.1159/000491999.
- Hodi FS, O’Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711-723. doi: 10.1056/NEJMoa1003466.
- Patnaik A, Kang SP, Rasco D, et al. Phase 1 study of pembrolizumab (MK-3475; anti-PD-1 monoclonal antibody) in patients with advanced solid tumors. Clin Cancer Res. 2015;21(19):4286-4293. doi: 10.1158/1078-0432. CCR-14-2607.
Although the data from these clinical trials on PRRT are valuable for guiding treatment decisions, additional trials are necessary that decouple SSAs from PRRT and generate evidence for the efficacy and safety of PRRT monotherapy. Clinicians generally feel comfortable combining SSAs with PRRT, but some question whether the SSA-PRRT combination (versus PRRT monotherapy) is ultimately necessary. Some clinicians prefer to treat according to methods from clinical trials and guidelines from NCCN, and they combine an SSA with PRRT to account for potential factors regarding PRRT that are not yet understood. However, others prefer to go off label and administer PRRT as a monotherapy to patients who are asymptomatic. Currently, PRRT as a monotherapy for GEP-NETs is being evaluated in the phase III, randomized, controlled COMPETE trial, with the experimental group receiving 177Lu-edotreotide and the control group receiving everolimus. The primary outcome is to demonstrate the efficacy of 177Lu-edotreotide in prolonging PFS in patients with progressive, inoperable, somatostatin receptor—positive GEP-NETs, and the secondary outcome is overall survival (OS) for these patients. Estimated primary completion date for this trial is December 2023.21