Publication
Article
Further Study and Tailored Treatments Remain Unmet Needs in Male Breast Cancer
Author(s):
Jose Pablo Leone, MD, discusses the distinguishing features of male breast cancer, explains the benefits and limitations of current treatments, and emphasizes the importance of raising awareness about this breast cancer subset to propel further research.
Jose Pablo Leone, MD

Breast cancer in men represents approximately 1% of all breast cancer diagnoses with approximately 2700 new cases per year in the United States.1
Unique risk factors have been indentified for this disease state, according to Jose Pablo Leone, MD. “Hereditary predisposition, particularly mutations in BRCA1 or BRCA2, with BRCA2 being one of the most common ones in men,” Leone said. “Other risk factors include smoking, excessive alcohol intake, inactivity, or obesity. One risk factor that is important in men is Klinefelter syndrome.”
In an interview with OncLive On Air®, Leone, director of the program for breast cancer in men and a senior physician at Dana-Farber Cancer Institute, as well as an assistant professor of medicine at Harvard Medical School in Boston, Massachusetts, discussed the distinguishing features of male breast cancer, explained the benefits and limitations of current treatments, and emphasized the importance of raising awareness about this breast cancer subset to propel further research.
What features of male breast cancer distinguish it from female breast cancer?
There are a number of unique features of breast cancer in men compared with women. For example, breast cancer is more commonly diagnosed at an older age in men compared with women. The median age of diagnosis is approximately 66 years compared with 59 or 60 years for women. [Additionally,] approximately 65% of breast cancers are estrogen receptor [ER] positive in women [unlike men]. The representation of the other subtypes particularly triple negative and ER-negative disease [are more prevalent in women]. Those 2 subtypes are particularly rare in men.
Because there are no [standard] screening programs men tend to be diagnosed with higher stage as compared with women. In terms of treatment, there are unique considerations, particularly with regards to hormonal therapy and the use of tamoxifen. Additional options that we have for women also include aromatase inhibitors in postmenopausal women. [We have to determine] optimal options for men. Those are the main things that differentiate the 2 [diseases].
Please expand on how the treatments for male breast cancer compare with those for female breast cancer and how certain treatments similarities might indicate the need for further specified research.
With the treatment of breast cancer in men, one of the challenges is that we have a lot less data than we do for women. There are, for example, no prospective randomized clinical trials on the local regional management of breast cancer for men meaning we don’t have any [clinically meaningful] data for this population.
[Data from] prospective randomized trials have demonstrated the role of breast conservation in men [as well as] the benefits of radiation in specific scenarios, such as after lumpectomy if a patient [receives a diagnosis] of node-positive breast cancer. So many of the [standard] recommendations are extrapolated from women, what do we know from women and the randomized trials that were done in women. With that there are also observational data supporting the use of those same recommendations in men, but even [those] data have limitations and weaknesses. So clearly, more research is needed to understand the best treatment options for [standard] treatment of breast cancer in men.
In terms of systemic therapies, tamoxifen is the main adjuvant endocrine therapy option for breast cancer in men. This is an area where we also need more research to understand what is the best endocrine therapy option for male breast cancer.
It may be that tamoxifen is the best to look into that option. But over the years we have learned that aromatase inhibitors have improved outcomes in postmenopausal women with breast cancer. And one wonders whether those may work equally well or even better than tamoxifen.
Another consideration is that, in premenopausal women, we know that the use of suppression with aromatase inhibitors improve outcomes beyond tamoxifen. And in men—particularly men who may present with higher stages of breast cancer—we don’t know whether using suppression in addition to either tamoxifen or aromatase inhibitor works better. We clearly need more studies done about the system therapy options that we have, including many that are already available.
This is also important because as the field continues to move forward, and we have more novel options available, many of those are being evaluated in women in combinations with aromatase inhibitors, which are drugs that we commonly don’t use as a single agent in men with breast cancer. So it is important to do studies in men to assess the efficacy.
In September 2022, a study you led was published in Cancer, looking at the efficacy of neoadjuvant chemotherapy in male breast cancer compared with female breast cancer. What did you find here?
That was a study that we did to evaluate the efficacy of neoadjuvant chemotherapy in men compared with women with breast cancer. To make the comparisons more clinically useful, we stratified the comparisons within tumor subtypes. We compared ER-positive [disease] with ER-negative disaese in men vs ER positive or negative disease in women within each tumor subtype. That study was done using data from National Comprehensive Cancer Network.
Overall, the rates of pathologic complete response in men were uniformly lower than in women with the same subtype [Table].2 Additionally, the likelihood of pathologic complete response was half in men than what we observed in women. It brings some hypotheses and some questions as to why that may be the case. Could it be that chemotherapy options were different between men and women? This could be one possibility where we can control for that. So what we did was narrow the duration of the chemotherapy, so that we could try to make the groups as homogeneous as possible.
Table. Outcomes With Neoadjuvant Chemotherapy in Men and Women With Breast Cancer2
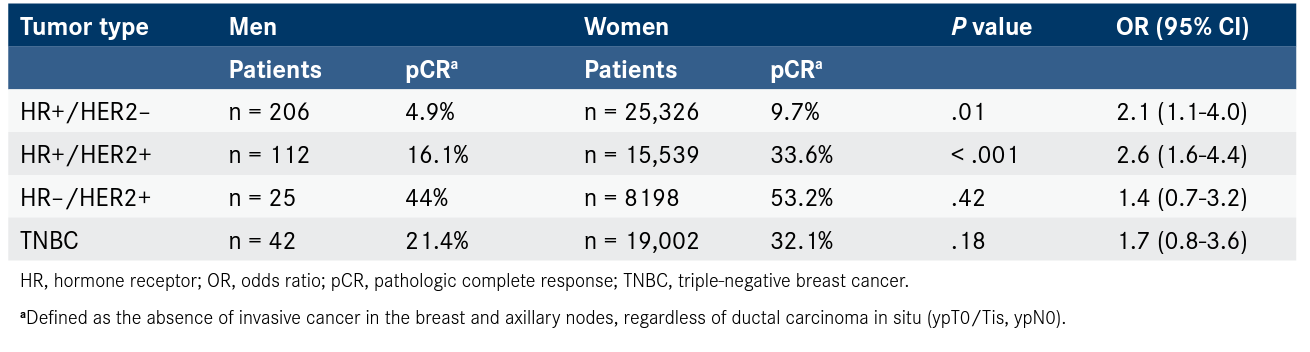
Another possibility may be that, biologically, breast cancer in men and females are different types of tumors. Male breast cancer may be more luminal than female breast cancer and may have a better benefit from a novel intervention as opposed to chemotherapy, for example. This may be evident across subtypes of breast cancer in men. So clearly, more research is necessary to understand the biologic implications of the different subtypes of breast cancer in men, and how those may be similar or different from female breast cancer.
We’ve talked a lot about the similarities and differences between male and female breast cancer. Would you say that there are potential benefits to enrolling patients with male breast cancer to clinical trials that are primarily studying female breast cancer? Or what other trial designs might be possible and beneficial for male breast cancer specifically?
It is very important for men to be enrolled in clinical trials, in general for breast cancer. And that can be done in one of 2 ways.
One way is to enroll men in general clinical trials that enroll both women or men, and that is something that has recently changed for the better, in my opinion, based on recommendations from the FDA, and from the American Society of Clinical Oncology, and also the National Cancer Institute. When we think about initiating a clinical trial for breast cancer, we’re thinking mostly about breast cancer in women. We have to think about what criteria are mentioned be eligible to participate. There may be a reason for which men should not participate, but there may also be a reason to include male subjects.
Historically, the inclusion exclusion criteria will say women with a diagnosis of breast cancer and again, sometimes that may be very appropriate, but sometimes it may not be and there may not be a need to exclude men. And so having the opportunity to enroll men on clinical trials that would otherwise enroll only women has 2 advantages in that scenario. One is that it allows men access to the same cutting edge new treatments that women will have access to. And on the other hand, it also allows that if sufficient number of men get them to enroll into those clinical trials, we may get information as to how effective those treatments are in men in the prospective design.
The other option that I was mentioning earlier is to conduct a clinical trial specifically focusing on male breast cancer, and that has its own advantages and disadvantages. One advantage is that the patients that you enrolled are all men, and therefore there will be less of a confounder if the effect of what we were testing was different between men and women. It may take longer to enroll clinical trials with these criteria but this disadvantage can be overcome by allowing the clinical trial to be opened up more sites across the United States or even the world.
There are many examples in oncology of many diseases that are as rare. In fact, it’s not even more rare than breast cancer that have successfully done prospective clinical trials evaluating treatments that are specific for those diseases. In breast cancer, we can do equally well, if not even better, and this is something that can be done.
Is there anything you’d like to add?
One additional thing to mention is that the previously discussed study also showed a role for pathologic complete response in male breast cancer. We know pathologic complete response is prognostic in women with breast cancer, we did not know whether it was prognostic in men and if it was by what amount or magnitude. And what we found in that study is that the role of pCR in men is prognostic in a similar manner to that of women. The men who achieved pathologic complete response have a similar good prognosis as women. Men who have residual disease have a similar worse prognosis, as compared with women who did not actually perform the response or have residual disease.
It is something that we think is helpful because it could promote the use of pathologic complete response potentially as a biomarker in clinical trials of male breast cancer depending on the strategy that we’re testing and the specific treatments that we’re considering. It it could be an end point to reconsider even the similarities in the prognosis that we have in comparison women.
References
- Key Statistics for breast cancer in men. American Cancer Society. Updated January 12, 2022. Accessed December 6, 2022. bit.ly/3F9Gef9
- Leone JP, Hassett MJ, Leone J, et al. Efficacy of neoadjuvant chemotherapy in male breast cancer compared with female breast cancer. Cancer. 2022;128(21):3796-3803. doi:10.1002/cncr.34448