Publication
Article
Therapeutic Vaccines Lead the Charge in HPV-Driven Cancers
Author(s):
The development of therapeutic vaccines for patients with cancers associated with the human papillomavirus has emerged as a leading strategy in continuing research efforts to address the growing public health threat posed by the virus.
The development of therapeutic vaccines for patients with cancers associated with the human papillomavirus (HPV) has emerged as a leading strategy in continuing research efforts to address the growing public health threat posed by the virus.
Although screening programs and prophylactic vaccines have helped curb infection and incidence rates of cervical cancer, the malignancy most definitively linked with HPV,1-3 the same cannot be said for other tumor types. Notably, oropharyngeal cancer (OPC) has now surpassed cervical cancer as the most common HPV-associated cancer.4
Meanwhile, poor HPV vaccine uptake and ineffective screening for cervical cancer, particularly in developing countries, has resulted in a pressing need to develop novel treatments.5,6
Figure 1. Elements of the HPV Genome6 (Click to Enlarge)
Slow and steady progress may win the day for the elimination of HPV-associated cancers, but open questions abound regarding the optimal management of these clinically and molecularly unique tumors.
A Common Virus
HPVs are double-stranded DNA viruses that encompass as many as 170 genotypes, according to current estimates. These viruses preferentially infect the squamous epithelium of skin and mucous membranes. Many infect the genital and oral areas, making HPV among the most common sexually transmitted viruses worldwide.7,10,11
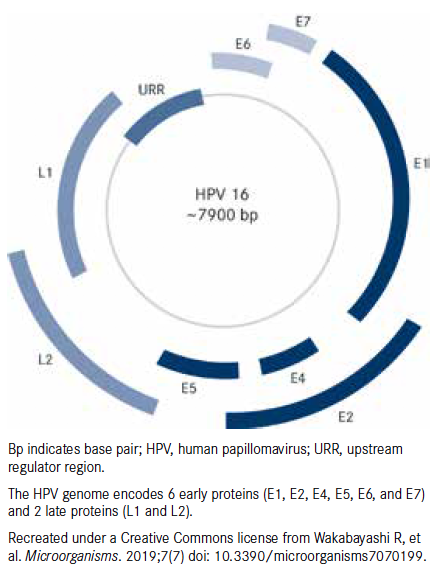
All HPV strains share a genome that encodes 8 proteins: the early proteins (E1, E2, E4, E5, E6 and E7), first to be expressed upon infection, and the late proteins (L1 and L2), structural proteins that make up the capsid surrounding the virus (Figure 16). The genome also contains an upstream region containing regulatory elements essential for the replication and transcription of viral DNA.7,10,11
Infection with HPV causes epithelial proliferation and the development of cutaneous warts, but several studies in the 1980s set the scene for the Nobel Prize—winning demonstration of a link between HPV infection and cervical cancer.10,12-14
Mucosal HPVs are now classified according to their potential carcinogenic risk. Low-risk HPVs, such as HPV6 and HPV11, are mainly linked to benign genital warts, while highrisk HPVs are associated with invasive cervical cancers.7,10,11 HPV16 and HPV18 are the most common high-risk HPVs and are responsible for about 70% of cervical cancer cases.15
In 2007, HPV was recognized as a risk factor for head and neck squamous cell carcinoma (HNSCC)16; in this case, HPV16 is the most prevalent type, accounting for almost 90% of cases.17 High-risk HPVs have subsequently been shown to be associated with a subset of anal, penile, vulvar, and vaginal cancers,18 and evidence suggests that HPV infections may contribute to the risk of prostate and lung cancers.19-21 Overall, HPV is thought to be responsible for about 5% of all cancers worldwide.11
Powerful Agent of Oncogenesis
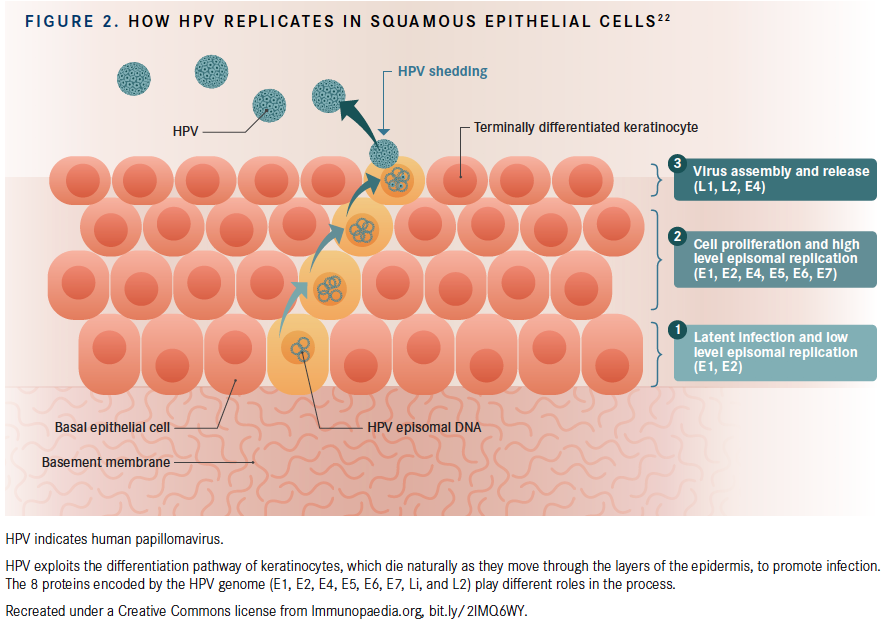
Our understanding of precisely how HPV causes cancer continues to evolve (Figure 222). In approximately 90% of cases, the immune system combats HPV infection and the virus becomes undetectable within 1 to 2 years. Initially, it was thought that the virus was completely eliminated, but some evidence suggests that it is merely kept in a state of latency.6
In a small percentage of cases, possibly as a result of a breakdown in the immune balance that keeps the virus suppressed, the infection persists and can drive cellular changes that cause the development of precancerous and, ultimately, cancerous lesions.6
The central drivers of HPV-induced oncogenesis are the E6 and E7 proteins, which are highly expressed in HPV-associated cancers. These proteins are directly involved in promoting cancerous transformation of host cells through their interactions with numerous downstream proteins, including the tumor suppressor proteins p53 and pRb, essentially reprogramming the basic functions of the cell.6,7,10,11
Another hallmark of HPV-associated cancer is the integration of viral DNA into the host genome; in contrast, the HPV genome is usually found in an episomal form in noncancerous host cells. The precise mechanisms by which integration occurs are not yet completely understood.6,11,18
The circular HPV DNA must break apart to integrate with the host genome, and studies have shown that the break points frequently occur in the region encoding the E2 gene, a transcriptional repressor of E6 and E7. Loss of E2 leads to overexpression of these 2 oncoproteins. Integration within the host DNA, which may not occur at entirely random sites, may foster genomic instability within the host genome, further driving carcinogenesis.6,11,17,23,24
Shifting Epidemiology
Thanks to a combination of cervical cancer screening and the development of prophylactic vaccines, the incidence of cervical cancer has been steadily declining over the past several decades.4
The FDA has approved 3 preventive HPV vaccines; however, only 1 is currently available in the United States. Gardasil 9, the successor to the quadrivalent vaccine Gardasil, targets 9 HPV types: 6, 11, 16, 18, 31, 33, 45, 52, and 58. These HPV types are responsible for 90% of cervical cancer cases.3 Since HPV vaccines hit the market, cervical cancer incidence has reportedly decreased by 29% among women aged 15 to 24 years.2
Meanwhile, the rates of HPV-associated OPC have been steadily increasing over a similar time frame, and this malignancy has now knocked cervical cancer off the top of the HPV-associated cancer pyramid.4
Despite the efficacy of HPV vaccination in preventing cervical cancer, less than half of adolescents in the United States were vaccinated by 2017,5 and less than 2% of females aged 9 to 45 years are vaccinated worldwide.6 Additionally, vaccine uptake and screening programs are rare in developing countries, where cervical cancer rates have remained high.6 Combined with the growing burden of HPV-associated OPC, HPV continues to present a substantial public health threat.
HPV-associated cancers have been found to be distinct from their HPV-negative counterparts with respect to histology, pathology, and clinical characteristics. Next-generation sequencing studies have also uncovered significant differences at the molecular level.25,26 Investigators believe there is a role for novel therapeutic strategies to address HPV-associated cancers.
The Promise of Vaccines
The L1 protein of HPV is able to assemble virus-like particles (VLPs) that morphologically resemble the HPV virion but contain no viral DNA. This was exploited for the design of current prophylactic vaccines that contain these VLPs, which are highly immunogenic and trigger the production of neutralizing antibodies by the host.27
Prophylactic HPV vaccines have been shown to confer long-term protection against infection,28,29 but since the capsid proteins are not expressed at detectable levels in infected or cancerous cells, these vaccines are not effective treatment options.7
(Click to Enlarge)
A variety of vaccine strategies have been tested and, although none have yet been approved by the FDA, we may be inching closer to that goal. Vaccine candidates dominate the novel approaches currently undergoing clinical testing for HPV-positive cancers (Table).
Live Vaccines
Live attenuated HPV vaccines have been produced by modifying a disease-producing bacterium or virus to secrete HPV proteins. Axalimogene filolisbac (ADXS11-001, AXAL; Advaxis), which was the lead vaccine candidate for several years, uses an attenuated version of the Listeria monocytogenes bacterium as a vector to secrete the HPV16 E7 protein fused to a fragment of listeriolysin O, the major virulence factor of this bacterium.33
ADXS11-001 was shown to be a highly effective and well-tolerated cervical cancer treatment in several phase II trials,34-36 including the GOG/NRG-0265 trial in which axalimogene monotherapy resulted in an unprecedented 1-year survival rate of 38% in patients with heavily pretreated recurrent metastatic cervical cancer.35
Based on these findings, phase III trials were initiated, including the AIM2CERV trial (NCT02853604), in which axalimogene was evaluated as adjuvant monotherapy in patients with locally advanced cervical cancer treated with chemoradiation therapy (CRT).
However, the past year has been a turbulent one for axalimogene. In January, the FDA placed a partial clinical hold on the AIM2CERV study as the agency sought additional information about chemistry, manufacturing, and control issues. Although the hold was subsequently lifted, Advaxis announced in June that the company was closing the trial for financial reasons. Although several other trials of axalimogene are ongoing, the company is reportedly planning to focus its resources on the development of next-generation vaccines.9,37
Viruses can also be used as vectors, and the modified vaccinia virus Ankara (MVA), an attenuated derivative of a poxvirus, has been the most widely used.7,10,30 In the tipapkinogen sovacivec vaccine, MVA expresses the HPV16 E6 and E7 proteins, in addition to interleukin (IL)-2, which serves as an adjuvant to boost vaccine potency.38
Table. Select Ongoing Clinical Trials in HPV-Positive Cancers (Click to Enlarge)
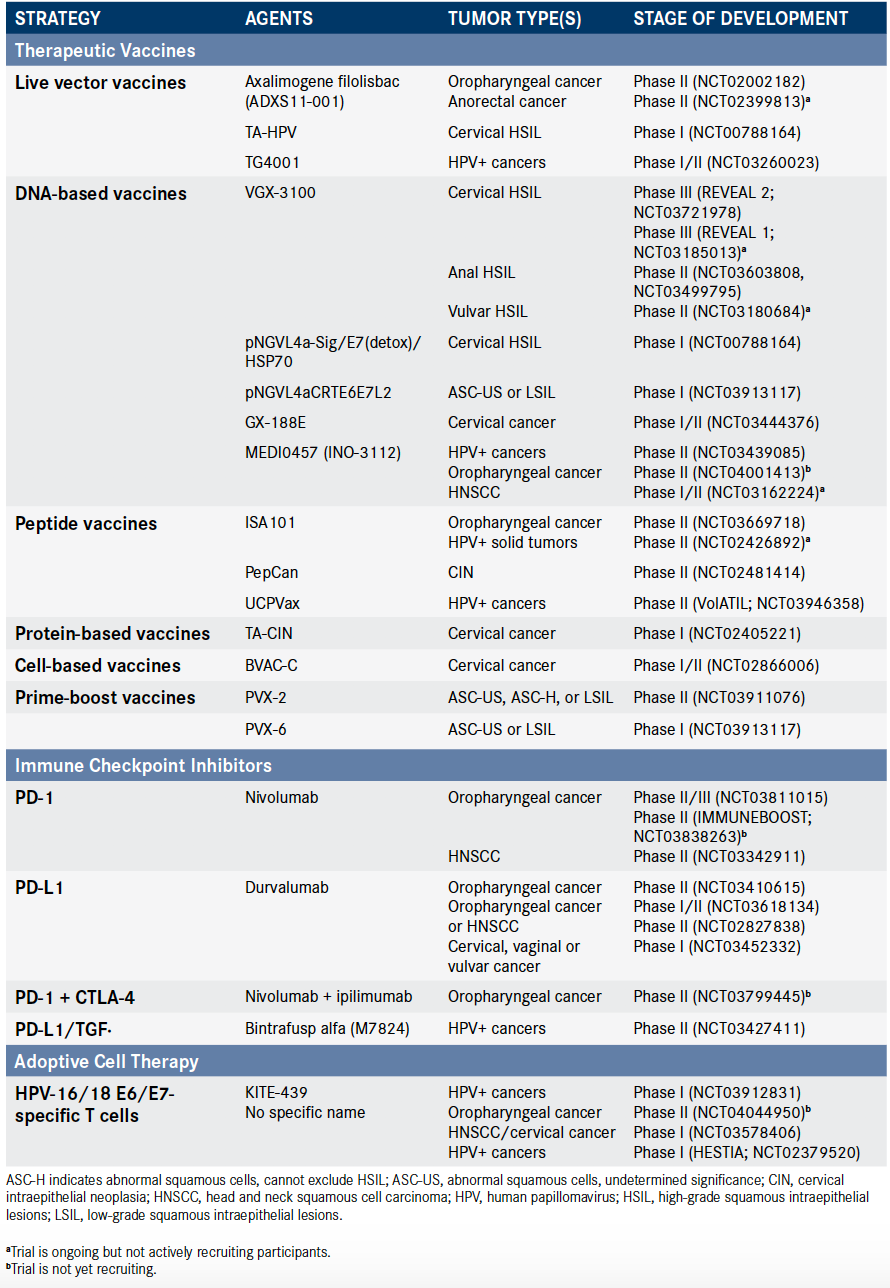
DNA-Based Vaccines
DNA vaccines are designed to use the genetic information encoding target antigens to elicit an immune response. They offer the advantage of being easier and cheaper to produce; they do not generate neutralizing antibodies as do live vaccines; and they can be administered more than once.7,10
VGX-3100, which Inovio Pharmaceuticals is developing, consists of a mixture of plasmids expressing a fusion of the E6 and E7 proteins of HPV16 and HPV18, offering the potential to target 2 high-risk HPV strains.10 In a phase II study, patients with grade 2/3 CIN (CIN2/3) associated with HPV16/18 were randomized to receive VGX-3100 (n = 125) or placebo (n = 42). In a per-protocol analysis, the histological regression rates were 49.5% versus 30.6%, respectively. The vaccine was well tolerated; only erythema was more common in vaccinetreated patients.39
Inovio is testing VGX-3100 against HPV-associated precancerous cervical, vulvar, and anal lesions. The most advanced program is in cervical precancer, where the phase III REVEAL 1 and REVEAL 2 trials are under way. Inovio recently reported that enrollment in the REVEAL 1 trial had been completed,8 making VGX-3100 among the most advanced vaccine candidates currently being evaluated in this arena.
Additional Vaccine Approaches
Other vaccination strategies being tested include peptide-based vaccines such as PepCan and ISA101 (ISA Pharmaceuticals). The latter uses synthetic long peptides (SLPs) derived from the E6 and E7 proteins to elicit an immune response.7 Once inside the patient, these SLPs are degraded to form shorter peptide epitopes by dendritic cells (DCs), the major antigen-presenting cells.40 In a phase I dose-escalation trial, in women with CIN2/3, PepCan elicited histological regression in 50% of patients, with no dose-limiting toxicities.41
BVAC-C is a DC-based vaccine based on B cells and monocytes that have been transfected with genes encoding recombinant HPV16/18 E6 and E7 proteins.7,42 Data presented at the 2018 European Society for Molecular Oncology Annual Meeting revealed that BVAC-C was well tolerated and had evidence of activity in patients with cervical cancer, consisting of 1 partial response (PR) and 4 patients with stable disease among 8 evaluable patients.42
Immune Checkpoint Inhibitors
HPVs have a complicated relationship with the immune system and have developed a multitude of mechanisms to avoid detection or tamp down the immune response that could affect vaccine efficacy. Rationally designed combination therapies are likely to be the most effective way to manage HPV-associated cancers, some investigators hypothesize.32
Expression of the immune checkpoint protein PD-1 and its ligand, PD-L1, which play a role in immune suppression, has been observed on T cells and DCs that infiltrate cervical tumors. Increased expression has been reported to correlate with high-risk HPV infection and increasing CIN grade.43,44
PD-1/PD-L1 blockade, utilizing the immune checkpoint inhibitors (ICIs) that have enjoyed significant success in other tumor types, could have potential in the treatment of HPV-associated cancers, particularly cervical cancer.
The PD-1 inhibitors pembrolizumab (Keytruda) and nivolumab (Opdivo) are approved for indications in cancers typically associated with HPV; however, these indications are not linked to HPV status.45,46 One ICI strategy moving forward involves testing these agents specifically in HPV-positive populations.
Approved Drugs
In June 2018, the FDA approved pembrolizumab for patients with recurrent or metastatic cervical cancer with disease progression on or after chemotherapy whose tumors express PD-L1. The approval was based on the results of the KEYNOTE-158 trial, in which the objective response rate (ORR) was 14.3% (95% CI, 7.4%-24.1%) among 77 patients with a combined positive score (CPS) ≥1 for PD-L1 expression, including a 2.6% complete response (CR) and an 11.7% PR rate. No responses were observed in patients with a CPS <1.45
Pembrolizumab is also approved as monotherapy in PD-L1—positive (CPS ≥1) patients and in combination with chemotherapy regardless of PD-L1 status as first-line treatment for metastatic HNSCC or for recurrent or unresectable disease based on results of the KEYNOTE-048 study.
In KEYNOTE-048, single-agent pembrolizumab improved median overall survival (OS) compared with the combination of cetuximab (Erbitux) plus chemotherapy for patients with CPS ≥1 (12.3 vs 10.3 months; HR, 0.78; P = .017) and CPS ≥20 (14.9 vs 10.7 months; HR, 0.61; P = .002). The combination of pembrolizumab and chemotherapy increased median OS to 13.0 months compared with 10.7 months for cetuximab plus chemotherapy (HR, 0.77; P = .007).45
Among patients with cancer of the oropharynx with CPS ≥20 who participated in the study, the combination of pembrolizumab plus chemotherapy improved OS compared with the cetuximab regimen for patients who were p16 positive (HR, 0.39) and those who p16 negative (HR, 0.66). Similarly, OS was also improved with the pembrolizumab regimen among those with CPS ≥1, with HRs of 0.55 and 0.69 for p16-positive and -negative disease, respectively. Investigators assessed p16 status with an immunohistochemistry (IHC) assay, with a 70% cutpoint for positivity.47
Additionally, nivolumab is approved for patients with recurrent or metastatic HNSCC based on findings from the CheckMate 141 study, in which nivolumab monotherapy demonstrated a median OS of 7.5 months compared with 5.1 months with investigator’s choice of chemotherapy (HR, 0.70; P = .01).48
In updated findings, the OS benefit of nivolumab was similar for patients with HPV-positive (HR, 0.63) and HPV-negative (HR, 0.64) disease. HPV status was also assessed through p16 IHC testing, with positivity defined as diffuse staining in ≥70% of cells.48,49
Investigational Agents
Bintrafusp alfa (M7824) is a novel kind of ICI, a fusion of a PD-L1—targeted antibody and the extracellular domain of transforming growth factor beta receptor II (TGFβR2), which acts as a trap for the immunosuppressive protein TGFβ.50,51
In a phase I clinical trial, 36 patients with HPV-associated cancers (4 anal, 18 cervical, and 14 HNSCC) were treated with escalating doses of M7824 every 2 weeks. The ORR was 27.8%, including 2 CRs and 8 PRs, with both CRs and 5 of 8 PRs ongoing at the time of presentation; 3 additional patients had a delayed PR after initial progression, according to findings presented at the 2019 American Association for Cancer Research Annual Meeting. Grade 3 treatment- related AEs included anemia, cystitis, and diabetic ketoacidosis.52
Combinations
Ongoing trials of ICIs are testing the efficacy of combining these agents with therapeutic vaccines. ISA101 has shown promise in combination with nivolumab; in a phase II clinical trial in patients with HPV-positive cancers, the ORR was 33% (8 of 24 patients, including 22 with OPC) and OS was 17.5 months. Grade 3/4 AEs requiring discontinuation of nivolumab occurred in 2 patients.53
Regulatory authorities in South Korea recently gave the go-ahead for a phase I/II clinical trial combining the DNA-based vaccine GX-188E with pembrolizumab in HPV-positive cervical cancer.54
Also under study is MEDI0457 (previously known as INO-3112), a DNA combination vaccine composed of VGX-3100 and INO-9012 (a DNA plasmid encoding the proinflammatory cytokine IL-12).55 MEDI0457 is being investigated in numerous ongoing phase II trials in combination with the PD-L1—targeting antibody durvalumab (Imfinzi).
Deintensifying Treatment?
Patients with HPV-positive HNSCC have a better prognosis than those whose disease is HPV-negative. HPV-positive HNSCC, with rapidly growing prevalence, is now recognized as a distinct clinical entity.56 In spite of this, both types of the disease are typically treated with a one-size-fits-all approach that can have serious long-term toxicity.
There is a growing consensus that patients with HPV-associated HNSCC might benefit from deintensified treatment in order to lessen the impact of toxicity while maintaining efficacy. However, the optimal means of achieving this remains controversial.57
One strategy is to replace cisplatin in CRT regimens with the EGFR-targeted monoclonal antibody cetuximab.58,59 EGFR is highly expressed in HNSCC, and cetuximab is approved for several indications in this cancer type.60
Unfortunately, the recently reported results of 2 clinical trials do not support the replacement of cisplatin with cetuximab as a deintensification strategy. The combination of cetuximab and radiation therapy did not improve toxicity and failed to meet the noninferiority criteria for OS in the RTOG 1016 study. In the De-ESCALaTE trial, the combination actually had a detrimental impact on tumor control, with significantly worse 2-year OS and recurrence.58,59
Although it is unclear whether clinical development of the tipapkinogen sovacivec vaccine will continue, the results of a phase II trial were recently reported. In patients with cervical intraepithelial neoplasia (CIN), a precancerous condition that can lead to cervical cancer, there was a greater rate of histological regression among vaccine-treated patients compared with those who did not receive treatment (18% vs 4%, respectively), resulting in a vaccine efficacy of 80%. It was well tolerated, with injection site reactions as the most common adverse event (AE).38
The development of novel therapeutic strategies has focused on a different kind of vaccine. Therapeutic vaccines are designed to stimulate cytotoxic T cell—mediated immune responses against HPV-infected cancer cells using viral antigens. The constitutively overexpressed E6 and E7 oncoproteins make the ideal target.30-32
To date, there has been major investment in the development of therapeutic vaccines designed to prime an antitumor immune response by exploiting oncogenic viral proteins.7 As the leading vaccine candidate, VGX-3100, moves closer to pivotal phase III clinical trial findings,8 the significant financial investment required to bring these drugs to fruition has left other once-promising drugs floundering.9
References
- Bosch FX, Lorincz A, Muñoz N, Meijer CJLM, Shah KV. The causal relation between human papillomavirus and cervical cancer. J Clin Pathol. 2002;55(4):244-265. doi: 10.1136/jcp.55.4.244.
- Guo F, Cofie LE, Berenson AB. Cervical cancer incidence in young U.S. females after human papillomavirus vaccine introduction. Am J Prev Med. 2018;55(2):197-204. doi: 10.1016/j.amepre.2018.03.013.
- Zhang S, Batur P. Human papillomavirus in 2019: an update on cervical cancer prevention and screening guidelines. Cleve Clin J Med. 2019;86(3):173-178. doi: 10.3949/ccjm.86a.18018.
- Van Dyne EA, Henley SJ, Saraiya M, Thomas CC, Markowitz LE, Benard VB. Trends in human papillomavirus-associated cancers - United States, 1999-2015. MMWR Morb Mortal Wkly Rep. 2018;67(33):918-924. doi: 10.15585/mmwr.mm6733a2.
- Walker TY, Elam-Evans LD, Yankey D, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 years - United States, 2017 [published correction appears in MMWR Morb Mortal Wkly Rep. 2018;67(41):1164. doi: 10.15585/mmwr.mm6741a8]. MMWR Morb Mortal Wkly Rep. 2018;67(33):909-917. doi: 10.15585/mmwr.mm6733a1.
- Wakabayashi R, Nakahama Y, Nguyen V, Espinoza JL. The host-microbe interplay in human papillomavirus-induced carcinogenesis. Microorganisms. 2019;7(7):e199. doi: 10.3390/microorganisms7070199.
- Chabeda A, Yanez RJR, Lamprecht R, Meyers AE, Rybicki EP, Hitzeroth II. Therapeutic vaccines for high-risk HPV-associated diseases. Papillomavirus Res. 2018;5:46-58. doi: 10.1016/j.pvr.2017.12.006.
- Inovio completes enrollment of VGX-3100 phase 3 trial (REVEAL 1) for the treatment of HPV-related cervical pre-cancer [news release]. Plymouth Meeting, PA: Inovio Pharmaceuticals, Inc; June 26, 2019. prnewswire.com/news-releases/inovio-completes-enrollment-of-vgx-3100-phase-3-trial-reveal-1-for-the-treatment-of-hpv-related-cervical-pre-cancer-300875373.html. Accessed August 25, 2019.
- Advaxis announces increasing focus on neoantigen-directed immunotherapies and closing of its phase 3 AIM2CERV study [news release]. Princeton, NJ: Advaxis, Inc; June 27, 2019. biospace.com/article/releases/advaxis-announces-increasing-focus-on-neoantigen-directed-immunotherapies-and-closing-of-its-phase-3-aim2cerv-study/. Accessed August 23, 2019.
- Almeida AM, Queiroz JA, Sousa F, Sousa Â. Cervical cancer and HPV infection: ongoing therapeutic research to counteract the action of E6 and E7 oncoproteins [published online August 6, 2019]. Drug Discov Today. doi: 10.1016/j.drudis.2019.07.011.
- Gupta S, Kumar P, Das BC. HPV: molecular pathways and targets. Curr Probl Cancer. 2018;42(2):161-174. doi: 10.1016/j.currproblcancer.2018.03.003.
- Dürst M, Gissmann L, Ikenberg H, zur Hausen H. A papillomavirus DNA from a cervical carcinoma and its prevalence in cancer biopsy samples from different geographic regions. Proc Natl Acad Sci U S A. 1983;80(12):3812-3815. doi: 10.1073/pnas.80.12.3812.
- Schwarz E, Freese UK, Gissmann L, et al. Structure and transcription of human papillomavirus sequences in cervical carcinoma cells. Nature. 1985;314(6006):111-114. doi: 10.1038/314111a0.
- zur Hausen H. Condylomata acuminata and human genital cancer. Cancer Res. 1976;36(2 pt 2):794.
- de Sanjose S, Quint WG, Alemany L, et al; Retrospective International Survey and HPV Time Trends Study Group. Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. Lancet Oncol. 2010;11(11):1048-1056. doi: 10.1016/S1470-2045(10)70230-8.
- Kobayashi K, Hisamatsu K, Suzui N, Hara A, Tomita H, Miyazaki T. A review of HPV-related head and neck cancer. J Clin Med. 2018;7(9):e241. doi: 10.3390/jcm7090241.
- Kreimer AR, Clifford GM, Boyle P, Franceschi S. Human papillomavirus types in head and neck squamous cell carcinomas worldwide: a systematic review. Cancer Epidemiol Biomarkers Prev. 2005;14(2):467-475. doi: 10.1158/1055-9965.EPI-04-0551.
- Ghittoni R, Accardi R, Chiocca S, Tommasino M. Role of human papillomaviruses in carcinogenesis. Ecancermedicalscience. 2015;9:526. doi: 10.3332/ecancer.2015.526.
- Bae JM, Kim EH. Human papillomavirus infection and risk of lung cancer in never-smokers and women: an ‘adaptive’ meta-analysis. Epidemiol Health. 2015;37:e2015052. doi: 10.4178/epih/e2015052.
- Hasegawa Y, Ando M, Kubo A, et al. Human papilloma virus in non-small cell lung cancer in never smokers: a systematic review of the literature. Lung Cancer. 2014;83(1):8-13. doi: 10.1016/j.lungcan.2013.10.002.
- Yang L, Xie S, Feng X, et al. Worldwide prevalence of human papillomavirus and relative risk of prostate cancer: a meta-analysis. Sci Rep. 2015;5:14667. doi: 10.1038/srep14667.
- Akagi K, Li J, Broutian TR, et al. Genome-wide analysis of HPV integration in human cancers reveals recurrent, focal genomic instability. Genome Res. 2014;24(2):185-199. doi: 10.1101/gr.164806.113.
- Akagi K, Li J, Broutian TR, et al. Genome-wide analysis of HPV integration in human cancers reveals recurrent, focal genomic instability. Genome Res. 2014;24(2):185-199. doi: 10.1101/gr.164806.113.
- Rusan M, Li YY, Hammerman PS. Genomic landscape of human papillomavirus-associated cancers. Clin Cancer Res. 2015;21(9):2009-2019. doi: 10.1158/1078-0432.CCR-14-1101.
- Pan C, Issaeva N, Yarbrough WG. HPV-driven oropharyngeal cancer: current knowledge of molecular biology and mechanisms of carcinogenesis. Cancers Head Neck. 2018;3:12. doi: 10.1186/s41199-018-0039-3.
- Weberpals JI, Lo B, Duciaume MM, et al. Vulvar squamous cell carcinoma (VSCC) as two diseases: HPV status identifies distinct mutational profiles including oncogenic fibroblast growth factor receptor 3. Clin Cancer Res. 2017;23(15):4501-4510. doi: 10.1158/1078-0432.CCR-16-3230.
- Ma B, Roden R, Wu TC. Current status of human papillomavirus vaccines. J Formos Med Assoc. 2010;109(7):481-483. doi: 10.1016/S0929-6646(10)60081-2.
- Naud PS, Roteli-Martins CM, De Carvalho NS, et al. Sustained efficacy, immunogenicity, and safety of the HPV-16/18 AS04-adjuvanted vaccine: final analysis of a long-term follow-up study up to 9.4 years post-vaccination. Hum Vacc Immunother. 2014;10(8):2147-2162. doi: 10.4161/hv.29532.
- Nygård M, Saah A, Munk C, et al. Evaluation of the long-term anti-human papillomavirus 6 (HPV6), 11, 16, and 18 immune responses generated by the quadrivalent HPV vaccine. Clin Vaccine Immunol. 2015;22(8):943-948. doi: 10.1128/cvi.00133-15.
- Su J-H, Wu A, Scotney E, et al. Immunotherapy for cervical cancer: research status and clinical potential. BioDrugs. 2010;24(2):109-129. doi: 10.2165/11532810-000000000-00000.
- Vora C, Gupta S. Targeted therapy in cervical cancer. ESMO Open. 2018;3(suppl 1):e000462. doi: 10.1136/esmoopen-2018-000462.
- Frazer IH, Chandra J. Immunotherapy for HPV associated cancer. Papillomavirus Res. 2019;8:100176. doi: 10.1016/j.pvr.2019.100176.
- Miles BA, Monk BJ, Safran HP. Mechanistic insights into ADXS11-001 human papillomavirus-associated cancer immunotherapy. Gynecol Oncol Res Pract. 2017;4:9. doi: 10.1186/s40661-017-0046-9.
- Basu P, Mehta A, Jain M, et al. A randomized phase 2 study of ADXS11-001 Listeria monocytogenes—Listeriolysin O immunotherapy with or without cisplatin in treatment of advanced cervical cancer. Int J Gynecol Cancer. 2018;28(4):764-772. doi: 10.1097/igc.0000000000001235.
- Huh W, Brady WE, Dizon DS, et al. A prospective phase II trial of the listeria-based human papillomavirus immunotherpay axalimogene filolisbac in second- and third-line metastatic cervical cancer: a NRG oncology group trial. Gynecol Oncol. 2017;145(suppl 1):220. doi: 10.1016/j.ygyno.2017.03.506.
- Petit RG, Mehta A, Jain M, et al. ADXS11-001 immunotherapy targeting HPV-E7: final results from a phase II study in Indian women with recurrent cervical cancer. J Immunother Cancer. 2014;2(suppl 3):92. doi: 10.1186/2051-1426-2-S3-P92.
- Advaxis’ phase 3 AIM2CERV study placed on partial clinical hold by FDA related to CMC requests [news release]. Princeton, NJ: Advaxis, Inc; January 23, 2019. ir.advaxis.com/press-release/advaxis-phase-3-aim2cerv-study-placed-partial-clinical-hold-fda-related-cmc. Accessed September 3, 2019.
- Harper DM, Nieminen P, Donders G, et al. The efficacy and safety of Tipapkinogen Sovacivec therapeutic HPV vaccine in cervical intraepithelial neoplasia grades 2 and 3: randomized controlled phase II trial with 2.5 years of follow-up. Gynecol Oncol. 2019;153(3):521-529. doi: 10.1016/j.ygyno.2019.03.250.
- Trimble CL, Morrow MP, Kraynyak KA, et al. Safety, efficacy, and immunogenicity of VGX-3100, a therapeutic synthetic DNA vaccine targeting human papillomavirus 16 and 18 E6 and E7 proteins for cervical intraepithelial neoplasia 2/3: a randomised, double-blind, placebo-controlled phase 2b trial. Lancet. 2015;386(10008):2078-2088. doi: 10.1016/s0140-6736(15)00239-1.
- NCI Drug Dictionary: synthetic long HPV16 E6/E7 peptides vaccine ISA101b (entry). National Cancer Institute website. cancer.gov/publications/dictionaries/cancer-drug/def/793552. Accessed August 25, 2019.
- Coleman HN, Greenfield WW, Stratton SL, et al. Human papillomavirus type 16 viral load is decreased following a therapeutic vaccination. Cancer Immunol Immunother. 2016;65(5):563-573. doi: 10.1007/s00262-016-1821-x.
- Choi CH, Choi HJ, Lee J-W, et al. Phase I study of BVAC-C in HPV type 16 or 18 positive recurrent cervical carcinoma: safety, clinical activity and immunologic correlates. Ann Oncol. 2018;29(suppl 8; abstract 960P). doi: 10.1093/annonc/mdy285.168.
- Karim R, Jordanova ES, Piersma SJ, et al. Tumor-expressed B7-H1 and B7-DC in relation to PD-1+ T-cell infiltration and survival of patients with cervical carcinoma. Clin Cancer Res. 2009;15(20):6341-6347. doi: 10.1158/1078-0432.CCR-09-1652.
- Yang W, Song Y, Lu YL, Sun JZ, Wang HW. Increased expression of programmed death (PD)-1 and its ligand PD-L1 correlates with impaired cell-mediated immunity in high-risk human papillomavirus-related cervical intraepithelial neoplasia. Immunology. 2013;139(4):513-522. doi: 10.1111/imm.12101.
- Keytruda [prescribing information]. Whitehouse Station, NJ: Merck & Co; 2019. www.accessdata.fda.gov/drugsatfda_docs/label/2019/125514s055s056lbl.pdf. Accessed September 3, 2019.
- Opdivo [prescribing information]. Princeton, NJ: Bristol-Myers Squibb; 2015. www.accessdata.fda.gov/drugsatfda_docs/label/2015/125527s000lbl.pdf. Accessed September 3, 2019.
- Rischin D, Harrington KJ, Greil R, et al. Protocol-specified final analysis of the phase 3 KEYNOTE-048 trial of pembrolizumab (pembro) as first-line therapy for recurrent/metastatic head and neck squamous cell carcinoma (R/M HNSCC). Presented at: 2019 American Society of Clinical Oncology Annual Meeting; May 31-June 4, 2019; Chicago, IL. Abstract 6000. meetinglibrary.asco.org/record/171051/abstract.
- Gillison ML, Blumenschein G Jr, Fayette J, et al. CheckMate 141: 1-year update and subgroup analysis of nivolumab as first-line therapy in patients with recurrent/metastatic head and neck cancer. Oncologist. 2018;23(9):1079-1082. doi: 10.1634/theoncologist.2017-0674.
- Ferris RL, Blumenschein G Jr, Fayette J, et al. Nivolumab for recurrent squamous-cell carcinoma of the head and neck. N Engl J Med. 2016;375(19):1856-1867. doi: 10.1056/NEJMoa1602252.
- GSK to co-develop Merck KGaA’s cancer immunotherapy candidate M7824 in $4.2B alliance. Genetic Engineering and Biotechnology News website. genengnews.com/news/gsk-to-co-develop-merck-kgaas-cancer-immunotherapy-candidate-m7824-in-4-2b-alliance/. Published February 5, 2019. Accessed August 26, 2019.
- Knudson KM, Hicks KC, Luo X,Chen JQ, Schlom J, Gameiro SR. M7824, a novel bifunctional anti-PD-L1/TGFβ trap fusion protein, promotes anti-tumor efficacy as monotherapy and in combination with vaccine [published correction appears in Oncoimmunology. 2019;8(5):e1584435. doi: 10.1080/2162402X.2019.1584435]. Oncoimmunology. 2018;7(5):e1426519. doi: 10.1080/2162402x.2018.1426519.
- Strauss J, Gatti-Mays ME, Cho B, et al. Phase I evaluation of M7824, a bifunctional fusion protein targeting TGF-β and PD-L1, in patients with human papillomavirus (HPV)-associated malignancies. Cancer Res. 2019;79(suppl 13; abstract CT075). doi: 10.1158/1538-7445.AM2019-CT075.
- Massarelli E, William W, Johnson F, et al. Combining immune checkpoint blockade and tumor-specific vaccine for patients with incurable human papillomavirus 16-related cancer: a phase 2 clinical trial. JAMA Oncol. 2019;5(1):67-73. doi: 10.1001/jamaoncol.2018.4051.
- Genexine receives approval to initiate phase Ib/II trial of GX-188E, HPV therapeutic DNA vaccine, in combination with Keytruda® (pembrolizumab), for the treatment of HPV-induced cervical cancer [news release]. Seongnam, South Korea: Genexine; June 19, 2017. businesswire.com/news/home/20170619005512/en/Genexine-Receives-Approval-Initiate-Phase-IbII-Trial. Accessed August 25, 2019.
- NCI Drug Dictionary: DNA plasmid-encoding interleukin-12/HPV DNA plasmids therapeutic vaccine MEDI0457 (entry). National Cancer Institute website. cancer.gov/publications/dictionaries/cancer-drug/def/775854. Accessed August 25, 2019.
- De Felice F, Tombolini V, Valentini V, et al. Advances in the management of HPV-related oropharyngeal cancer. J Oncol. 2019;2019:9173729-9173729. doi: 10.1155/2019/9173729.
- Kelly JR, Husain ZA, Burtness B. Treatment de-intensification strategies for head and neck cancer. Eur J Cancer. 2016;68:125-133. doi: 10.1016/j.ejca.2016.09.006.
- Gillison ML, Trotti AM, Harris J, et al. Radiotherapy plus cetuximab or cisplatin in human papillomavirus-positive oropharyngeal cancer (NRG Oncology RTOG 1016): a randomised, multicentre, non-inferiority trial. Lancet. 2019;393(10166):40-50. doi: 10.1016/s0140-6736(18)32779-x.
- Mehanna H, Robinson M, Hartley A, et al; De-ESCALaTE HPV Trial Group. Radiotherapy plus cisplatin or cetuximab in low-risk human papillomavirus-positive oropharyngeal cancer (De-ESCALaTE HPV): an open-label randomised controlled phase 3 trial. Lancet 2019;393(10166):51-60. doi: 10.1016/s0140-6736(18)32752-1.
- Chapman CH, Saba NF, Yom SS. Targeting epidermal growth factor receptor for head and neck squamous cell carcinoma: still lost in translation? Ann Transl Med. 2016;4(4):80. doi: 10.3978/j.ssn.2305-5839.2016.01.01.