Lung Cancer
Latest News

Latest Videos

CME Content
More News

Treatment in lung cancer continues to evolve at a rapid pace with the arrival of a set of efficacious new agents and promising evidence-based data. According to Corey J. Langer, MD, a veritable avalanche of additional data is on the way.

Mark G. Kris, MD, medical oncologist, Memorial Sloan Kettering Cancer Center, discusses challenges associated with sequencing in the treatment of patients with lung cancer.

It has been about 18 months since the first immunotherapy checkpoint agent was approved for patients with non–small cell lung cancer. Now there are 3 monoclonal antibodies that target the PD-1/PD-L1 pathway on the market for the tumor type and the focus has shifted rapidly to establishng immunotherapy as a new frontline standard.

Sonja Althammer, PhD, Team Leader Bioinformatics at Definiens, Munich, Bavaria, Germany, discusses a study looking to define a subgroup of patients with non–small cell lung cancer (NSCLC) who respond well to treatment with the PD-L1 inhibitor durvalumab.

The expression of PD-L1 has been at the forefront of biomarker development for PD-1/PD-L1 inhibitors, but there is much uncertainty surrounding its use and other biomarkers are needed.

Sarah B. Goldberg, MD, MPH, assistant professor of Medicine, Yale Cancer Center, discusses the use of PD-L1 as a biomarker in treating patients with lung cancer.

Hossein Borghaei, DO, chief, Division of Thoracic Medical Oncology, director, Lung Cancer Risk Assessment, associate professor, Department of Hematology/Oncology, Fox Chase Cancer Center, discusses the management of slightly rarer side effects that patients with lung cancer can experience when treated with immunotherapy agents.

Recent research suggests that the presence of PD-L1–positive and CD8+ cells may be useful for predicting responses in patients with non-small cell lung cancer who have been treated with durvalumab.

A biologics license application (BLA) has been submitted for ABP-215, a biosimilar version of bevacizumab (Avastin), based on data from analytical, pharmacokinetic, clinical data, pharmacology, and toxicology data, according to a statement from Amgen and Allergan, the developers of the biosimilar.

Immunotherapy continues to revolutionize the field of non–small cell lung cancer, with researchers now focusing on the optimal use of immune agents in the frontline setting.
Hossein Borghaei, DO, discuss what lies ahead for immunotherapy in lung cancer, and what changes may be on the horizon for such agents as pembrolizumab (Keytruda), nivolumab (Opdivo), and ipilimumab (Yervoy) in the frontline setting.

Balazs Halmos, MD, director, Thoracic Oncology, director, Clinical Cancer Genomics, Montefiore Medical Center, discusses the prevalence of MET mutations in patients with non–small cell lung cancer (NSCLC).

H. Jack West, MD, a thoracic oncologist of Swedish Cancer Institute at Swedish Medical Center, discusses factors he takes into consideration for EGFR tyrosine kinase inhibitors in patients who have EGFR-positive non–small cell lung cancer (NSCLC).
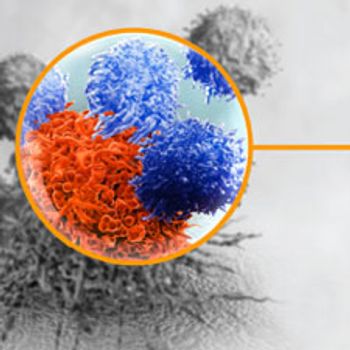
Immuno-oncology is among the most discussed topics in cancer research, but many are unaware of the science behind this class of treatments. Learn how it works.

Individualizing frontline therapy for patients with non–small cell lung cancer based on preferences and clinical experience, as well as efficacy and safety data from pivotal trials, is an appropriate method for selecting EGFR-targeted agents.

The treatment landscape for patients with ALK-rearranged non–small cell lung cancer is changing rapidly, gearing up the potential for more therapeutic options to address the heterogeneity of the mechanism of resistance in this population.

Roman Perez-Soler, MD, chairman of the Department of Oncology and chief of the Division of Medical Oncology at Montefiore Medical Center, Albert Einstein College of Medicine of Yeshiva University, discusses the impact of osimertinib (Tagrisso) on patients with T790M-positive non–small cell lung cancer (NSCLC).

Anne Chiang, MD, PhD, professor and thoracic oncologist at Yale Cancer Center, discusses molecular testing in lung cancer and how it affects treatment decisions.