JAK Inhibitors Used as Anti-inflammatory Therapeutics for Pancreatic Cancer
Experts review ongoing clinical research with JAK inhibitors in advanced pancreatic cancer as well as some strategies for preclinical testing of vertical inhibition of the JAK pathway.
Abstract
Pancreatic cancer will be second only to lung cancer as the most common cause of death from cancer in US by 2030. Most patients are diagnosed with unresectable disease. In this setting, novel combinations of cytotoxics such as FOLFIRINOX and nab-paclitaxel plus gemcitabine have led to modest improvements in survival. At the time of disease progression, less than 50% of the patients will be fit to receive second-line therapy. Patients with advanced pancreatic cancer often develop debilitating cachexia. It is hypothesized that the disease induces a systemic inflammatory response following cytokine production mediated by cancer cells or stromal cells. Plasma levels of biomarkers associated with inflammation, such as C-reactive protein, have also been associated with poor outcomes in patients with advanced pancreatic cancer. The Jak/Stat pathway plays a key role in driving this inflammatory response. Janus kinases are the main signaling transducers for cytokine receptors. Activated Jak recruits and activates transcription factors (Stat) and different signaling pathways including Src, Ras, and the PI3K/Akt pathway. Jak inhibitors may inhibit cancer cell proliferation by disrupting these signaling pathways. Jak inhibitors may also impair the systemic inflammatory response underlying the development of cachexia. A randomized phase 2 trial recently failed to show a benefit in survival when ruxolitinib, a Jak2 inhibitor, was added to capecitabine in the second line. However, in a prespecified subset analysis, a modest improvement in survival was seen in patients with elevated C-reactive protein at baseline. Two randomized phase 3 trials are currently testing ruxolitinib in combination with capecitabine in patients with advanced pancreatic cancer. Patients must have elevated C-reactive protein at baseline to be eligible to participate in this study. In addition, a number of immune modulators are under development or have gained regulatory approval for different indications. This work will review ongoing clinical research with Jak inhibitors in advanced pancreatic cancer as well as some strategies for preclinical testing of vertical inhibition of the Jak pathway.
Introduction
Pancreatic ductal adenocarcinoma (PDA) is the fourth most common cause of death from cancer in the United States. It is projected that by 2030 it will be second only to NSCLC as the leading cause of cancer related mortality in US.1 In 2015, 48,960 new cases will be diagnosed in the United States, and 40,560 patients will succumb to the disease.2 The overall 5-year survival rate is less than 5%.3 Therefore, novel treatments are urgently needed in this disease. Recent data from a randomized phase 2 trial showed that a subset of patients with PDA may benefit from targeting the Janus kinase pathway.4 Janus kinases (Jak) are the main signaling transducers for cytokine receptors. Cytokines regulate immune response and inflammation. They also play a role in oncogenesis.5 Four different non-receptor tyrosine Jaks (Jak1, Jak2, Jak3 and Tyk2) have been identified.6 Jak family members contain seven conserved JAK homology (JH) domains. JH1 and JH2 are composed of almost identical phosphate transferring domains, a kinase and pseudokinase domain. The JH2, or pseudokinase domain, is catalytically active and can phosphorylate the kinase domain (JH1).7 JH3-7 are characterized by N-terminal regions or sites of interaction with cytokine receptors. Tyk2 was the first member of the JAK family to be isolated.8 Inactivation of Tyk2 in mice decreased response to interferon-alpha/beta (IFNÉ‘/β), IL-12 and led to defective Stat3 activation.9 Homozygous Tyk2 mutations cause autosomal recessive hyper-IgE syndrome, a rare primary immunodeficiency disorder characterized by repeated staphylococcal skin infections, respiratory infections, and elevated levels of IgE.10 Jak1 is a signal transducer for IFNÉ‘/β, IFN-γ, IL-2, IL-4, IL-6, IL-7, IL-9, IL-15, and IL-21. Mice that have a Jak1 deficiency die perinatally.11 Jak2 is critical for signaling by IFNÉ‘/β, IL-3, IL-5, granulocyte-macrophage colony-stimulating factor (GM-CSF), erythropoietin (EPO), and growth hormone (GH). Its kinase activity, rather than its non-kinase status, is essential for mammalian development.12 The critical role of Jak2 in hematopoiesis was initially elucidated in Jak2-deficient mice models more than 20 years ago.13,14 In those models, Jak2-deficient embryos were characterized by an absence of red blood cells in the liver indicating impairment of liver hematopoiesis.
No JAK2 mutant embryos were detected beyond 10-12 days, demonstrating that, during that stage of their development, impairment of liver hematopoiesis was lethal. In addition, the response to other cytokines such as GM-CSF, IL-3, and IL-5 was also impaired in Jak2-deficient embryos.13 Lastly, Jak3 is primarily expressed in cells of the immune system.15 Mutations in JAK3 have been identified in patients with autosomal recessive severe combined immunodeficiency (SCID).16
Jaks are activated after binding to a dimerized cytokine or growth factor receptor (ie, IL-6, interferon, EPO, or GMCSF receptor). Activated Jak recruits and activates transcription factors (Stat) and different signaling pathways (Src, RAS and the PI3K-AKT pathway).6 Upon activation, Stat dimers translocate to the nucleus to initiate transcription of target genes involved in cell proliferation (Figure).17 Stat1 is the main transcriptional mediator of IFN. It can also be activated through IL-6. It regulates innate and adaptive immune responses. Stat1 deficiency in humans increases susceptibility to infections by mycobacteria and recurrent encephalitis secondary to herpes simplex virus type-1 (HSV-1).18 Stat3 can be activated by different cytokines (IL-6, IL-10, G-CSF) as well as receptor tyrosine kinases (ie, MET, EGFR) and non-receptor TK (Src). Stat3 is also required for G-CSF induced expansion of granulocytes. Ablation of Stat3 leads to embryonic lethality.19
Role of the JAK/STAT Pathway in Cancer
Activation of the JAK/STAT pathway occurs through aberrations in different components of the pathway including autocrine/ paracrine cytokine production, activating mutations of receptors or downstream transducers such as JAK and, finally, activating mutations in STAT (Figure). Levels of pStat3 are higher at the invasive margin of tumors, which suggests paracrine activation by stromal cells. Indeed, in different tumor types, cancer-associated fibroblasts are a source of IL-6, a cytokine receptor ligand.20,21 Constitutive activation of the JAK/STAT pathway has been reported in different proliferative disorders. Activating mutations within the JH2 pseudokinase domain (JAK2 V617F) disrupts the auto-inhibitory activity of JH2 and leads to constitutive activation of the kinase domain (JH1). JAK2 V617F mutations are present in more than 95% of patients with polycythemia vera as well as in more than 50% of patients with essential thrombocythemia or myelofibrosis.22 In patients with myelofibrosis, ruxolitinib (Jak1/2 inhibitor) resulted in improved overall survival and gained FDA-approval in 2011 for that disorder.23 Of note, a decrease in inflammatory cytokines (TNF-É‘, IL-6 and C-reactive protein) also occurred in response to ruxolitinib. Hematologic toxicity, including grade 3/4 anemia (45%), thrombocytopenia (13%) and neutropenia (7%), was commonly seen. Somatic mutations in JAK2 have been reported in 9% of patients with B-cell acute lymphoblastic leukemia (ALL).24 Activating JAK1 mutations are present in some patients with T-cell ALL as well as acute myeloid leukemia.25,26
Activating mutations in MPL, which codes for the thrombopoietin receptor, are found in 9% of patients with myelofibrosis in the absence of JAK2 V617F mutations.27 Other cytokine receptors (CRLF2) can be overexpressed as a result of chromosomal rearrangements in high-risk children with B-cell ALL.28 Mutations in STAT3 are reported in 40% of patients with large granular leukemias as well as ABC diffuse large-B-cell lymphoma, nasopharyngeal and breast cancer.29
Lastly, non-canonical pathway activation secondary to epigenetic modifications has also been reported. Jak2 can translocate to the nucleus and phosphorylate tyrosine 41 on the histone H3 tail. This prevents binding of heterochromatin protein 1É‘ (HP1É‘ is required for heterochromatin formation).30 Disrupting heterochromatin formation promotes expression of transcription factors such as Myc.31
JAK/STAT Activation in Pancreatic Cancer
Several lines of evidence suggest a role for inflammation in oncogenesis in pancreatic ductal adenocarcinoma (PDA). Chronic inflammation of the pancreas (pancreatitis) increases the risk of developing pancreatic cancer.32,33 The role of inflammation in PDA development has also been demonstrated in preclinical models. In a KRAS G12V mouse model, induction of chronic pancreatitis was necessary for PDA development during adulthood.34
Moreover, IL-6-mediated Stat3 activation is required for progression from premalignant PanIN lesions to PDA in mice with KRAS G12D mutations. Inflammatory cytokines such as IL-6 contribute to the immunosuppressive role of the stroma through expansion of myeloid-derived suppressor cells (MDSCs).35
In patients with resected PDA, JAK/STAT pathway activation was associated with a poor outcome.36 Lastly, plasma levels of biomarkers associated with inflammation, such as C-reactive protein (CRP), have also been associated with poor outcomes in patients with advanced PDA.37 It is hypothesized that PDA induces a systemic inflammatory response following cytokine production mediated by cancer cells or stromal cells. JAK/STAT-dependent cytokine signaling drives this inflammatory response.38 Together with complications from PDA such as gastrointestinal obstruction, ascites or pancreatic insufficiency, this systemic inflammatory response is largely responsible for the cachexia characteristic of the disease.39
The mechanism of JAK/STAT activation in PDA remains to be elucidated. Genomic analysis in a small series of 26 pancreatic cancer patients did not find oncogenic JAK V617F mutations.40 The Washington University group recently reported a JAK2 mutation (2964 G>C) in a pancreatic cancer patient.41 However, the mutation was predicted to be neutral. A search in the cBio- Portal for Cancer Genomics (www.cbioportal.org, data accessed on 2/25/2015) identified genetic aberrations in JAK2 in 2% of samples from patients with pancreatic cancer (n=90).42 A JAK2 S602I missense mutation and a JAK2 R443* nonsense mutation were found in one of the patients. Amplification in JAK2 (9p24) was reported in a different patient. Mutations in JAK1, most commonly truncating mutations, were present in 8% of samples. A missense mutation in JAK3 G712S was also identified in one patient.
Figure.
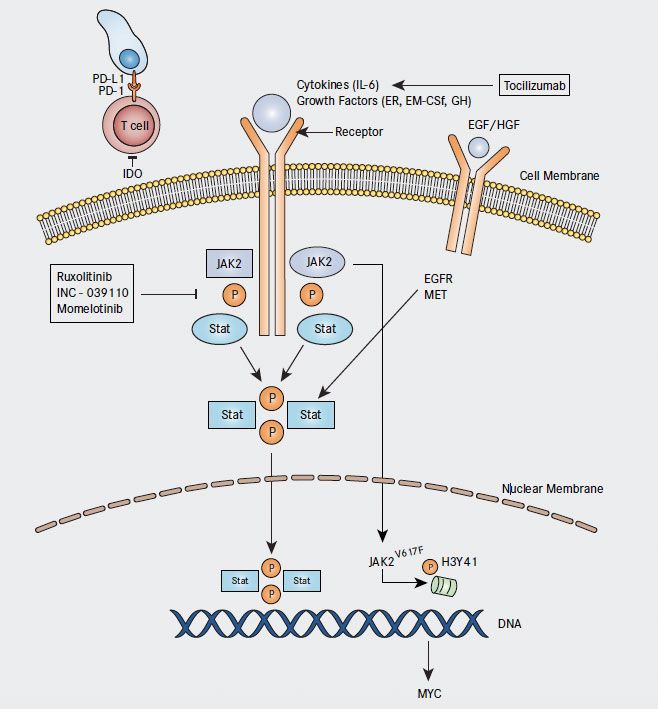
The Janus kinase pathway may be activated as a result of 1) Autocrine/Paracrine cytokine production 2) Activating mutations of cytokine receptors or JAK and 3) Activating mutations in STAT. Preclinical studies testing vertical inhibition of the pathway or combination of JAK inhibitors with different immunotherapies (IDO or checkpoint inhibitors) are needed to elucidate the role of JAK2 inhibition in the treatment of PDA.
TYK2 missense mutations (V318L and R607H) are present in 2% of samples. Overall, JAK mutations are reported in approximately 1-2% of patients with PDA. While JAK2 V617F mutations are predictive of response to Jak inhibitors in patients with myelofibrosis, there is no evidence yet that a JAK2 mutation will be predictive of response to Jak inhibitors in PDA.
Finally, it is also possible that genetic aberrations other than oncogenic mutations in JAK2 mediate STAT pathway activation in this disease. Indeed, high-throughput gene expression analysis has also found JAK2 enrichment in immune response pathways including JAK-STAT in PDA.43 Preclinical work in pancreatic cancer cell lines suggests that increased expression of gp130 and p-STAT3 may predict response to Jak2 inhibitors in this disease.44
Targeting the JAK/STAT Pathway in PDA
Ruxolitinib (INC424) is a Jak 1/2 inhibitor currently undergoing clinical testing in patients with advanced pancreatic cancer. The results of a second-line randomized phase 2 trial with capecitabine plus ruxolitinib or placebo in patients with metastatic pancreatic cancer (RECAP trial) were recently presented at ASCO.4 The study enrolled patients with a Karnofsky score of PS ≥60 who had disease progression with gemcitabine. The study was negative for its primary endpoint (overall survival in an intention-to-treat analysis). However, in a prespecified subset analysis, patients with serum CRP >13mg/L had an improvement in the 6-month survival rate (6mSR; 42% vs. 11%, HR=0.47, P = .01). Treatment was well tolerated. In general, the incidence of adverse events was similar in both groups. The incidence of pulmonary embolism (12% vs. 5%) as well as grade 3-4 anemia (15% vs. 2%) was increased in the ruxolitinib group. A larger number of patients in the ruxolitinib arm experienced weight gain (defined as a gain > 5% of baseline weight) not related to ascites or edema. This finding suggests Jak inhibitors might also be effective anticachexia drugs. It is hypothesized that selection of patients with increased CRP levels will enrich trials with patients likely to benefit from this Jak inhibitor. Two randomized phase 3 trials, JANUS1 (NCT02117479) and JANUS2 (NCT02119663) are currently evaluating capecitabine in combination with ruxolitinib or placebo in patients with advanced PDA and a level of CRP >10mg/L (Table 1).45,46 Two phase 1b studies are testing different Jak 1/2 inhibitors (ruxolitinib or momelotinib [GS-0387]) in combination with nab-paclitaxel and gemcitabine in advanced PDA.47 48 Jak inhibitors that preferentially target Jak1 are also undergoing clinical evaluation. INCB039110 (Jak1 inhibitor) is currently in being studied in a phase 1b clinical trial in combination with nab-paclitaxel plus gemcitabine in patients with advanced solid tumors.49 This trial will have a dose expansion cohort limited to patients with advanced PDA.
Table 1. Ongoing Clinical Trials With Jak Inhibitors in Metastatic Pancreatic Cancer
ABI indicates nab-paclitaxel; CAPOX, capecitabine plus oxaliplatin; RP2, randomized phase 2
Opportunities for Vertical Inhibition of an Inflammation Pathway in PDA
The portfolio of drugs targeting inflammation is increasing rapidly and, therefore, various opportunities to develop combinations of targeted anti-inflammatory drugs are now available (Table 2). Early clinical trials with targeted therapy have recently shown that horizontal inhibition of different pathways is unlikely to be successful due to increased toxicity, which limits achieving optimal biological doses.50,51 In contrast to this, vertical inhibition of different signal transducers in a single pathway have proven successful.52,53 Vertical inhibition of the JAK/Stat pathway needs to be tested in preclinical models. This can include a combination of monoclonal antibodies against IL-6 or its receptor plus Jak inhibitors (Table 2). In addition, monoclonal antibodies against colony stimulating factor 1 receptor (CSF1R) are undergoing clinical evaluation and offer additional opportunities to test vertical inhibition of the Jak pathway. Some cytotoxic agents (5-FU) inhibit MDSC and are currently being tested in combination with JAK inhibitors. Monoclonal antibodies against CXCR4 inhibit recruitment of immature myeloid cells to the tumor and could also be tested in preclinical models in combination with JAK inhibitors.
Table 2. Potential Partners for Preclinical Testing of Vertical Inhibition in Combination With Jak Inhibitors
mAb indicates monoclonal antibody
Lastly, novel strategies including testing drugs in patients at earlier stages of disease also need to be evaluated. In this regard, a recent phase 1b dose escalation study showed that testing immunotherapies in the neoadjuvant setting is feasible and safe.54 In this trial, patients were treated with FOLFIRINOX in combination with PF- 04136309 (a monoclonal antibody against CCR2, which depletes tumor-associated macrophages [TAM]). The high response rate (52%) was encouraging.
In conclusion, several lines of evidence support a role for inflammation in oncogenesis in PDA. This inflammatory response seems to be driven by JAK/STAT pathway. Jak inhibitors hold promise in a subset of PDA patients with elevated CRP. Additional preclinical work is needed to test whether vertical inhibition of the pathway will be an effective strategy.
About the Author
Author affiliation: Departments of Internal Medicine (Division of Oncology) and Center for Investigational Therapeutics, Huntsman Cancer Institute, University of Utah, Salt Lake City.
Corresponding author: Ignacio Garrido-Laguna, MD, PhD, Assistant Professor, GI Oncology/Phase 1 Program, Department of Internal Medicine, Oncology Division, University of Utah School of Medicine, Huntsman Cancer Institute, 2000 Circle of Hope, Suite 2100, Salt Lake City, UT 84112, Phone: 801-585-0255, Fax: 801-585-0124. E-mail: ignacio.garrido-laguna@hci.utah.edu.
References
- Rahib L, Smith BD, Aizenberg R, et al. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014;74:2913-2921.
- Siegel RL, Miller KD, Jemal A: Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5-29.
- Hidalgo M: Pancreatic cancer. N Engl J Med. 2010;362:1605-1617.
- Hurwitz H, Uppal, N., Wagner, S.A et al. A randomized double-blind phase 2 study of ruxolitinib or placebo with capecitabine as second-line therapy in patients with metastatic pancreatic cancer. Presented at: ASCO Annual Meeting. J Clin Oncol. 2014 Abstracts, vol 32, No 15, suppl (May 20 Supplement): 4000.
- Hirano T, Ishihara K, Hibi M: Roles of STAT3 in mediating the cell growth, differentiation and survival signals relayed through the IL-6 family of cytokine receptors. Oncogene. 2000;19:2548-2556.
- Rane SG, Reddy EP: Janus kinases: components of multiple signaling pathways. Oncogene. 2000;19:5662-5679.
- Bandaranayake RM, Ungureanu D, Shan Y, et al. Crystal structures of the JAK2 pseudokinase domain and the pathogenic mutant V617F. Nat Struct Mol Biol. 2012;19:754-759.
- Firmbach-Kraft I, Byers M, Shows T, et al. Tyk2, prototype of a novel class of non-receptor tyrosine kinase genes. Oncogene. 1990;5:1329-1336.
- Karaghiosoff M, Neubauer H, Lassnig C, et al. Partial impairment of cytokine responses in Tyk2-deficient mice. Immunity. 2000;13:549-560.
- Minegishi Y, Saito M, Morio T, et al. Human tyrosine kinase 2 deficiency reveals its requisite roles in multiple cytokine signals involved in innate and acquired immunity. Immunity; 25:745-755.
- Rodig SJ, Meraz MA, White JM, et al. Disruption of the Jak1 gene demonstrates obligatory and nonredundant roles of the Jaks in cytokine-induced biologic responses. Cell. 1998;93:373-383.
- Frenzel K, Wallace TA, McDoom I, et al. A functional Jak2 tyrosine kinase domain is essential for mouse development. Exp Cell Res. 2006; 312:2735-2744.
- Parganas E, Wang D, Stravopodis D, et al. Jak2 is essential for signaling through a variety of cytokine receptors. Cell. 1998;93:385-395.
- Neubauer H, Cumano A, Muller M, et al. Jak2 deficiency defines an essential developmental checkpoint in definitive hematopoiesis. Cell. 1998;93:397-409.
- Johnston JA, Kawamura M, Kirken RA, et al. Phosphorylation and activation of the Jak-3 Janus kinase in response to interleukin-2. Nature. 1994;370:151-153.
- Macchi P, Villa A, Giliani S, et al. Mutations of Jak-3 gene in patients with autosomal severe combined immune deficiency (SCID). Nature. 1995;377:65-68.
- Quintas-Cardama A, Verstovsek S. Molecular pathways: Jak/STAT pathway: mutations, inhibitors, and resistance. Clin Cancer Res. 2013;19:1933-1940.
- Dupuis S, Jouanguy E, Al-Hajjar S, et al. Impaired response to interferonalpha/ beta and lethal viral disease in human STAT1 deficiency. Nat Genet. 2003;33:388-391.
- Takeda K, Noguchi K, Shi W, et al. Targeted disruption of the mouse Stat3 gene leads to early embryonic lethality. Proc Natl Acad Sci U S A. 1997;94:3801-3804.
- Sun X, Mao Y, Wang J, et al. IL-6 secreted by cancer-associated fibroblasts induces tamoxifen resistance in luminal breast cancer. Oncogene, 2014 Jun 9. doi: 10.1038/onc.2014.158. Epub 2014 Jun 9.
- Nagasaki T, Hara M, Nakanishi H, et al. Interleukin-6 released by colon cancer-associated fibroblasts is critical for tumour angiogenesis: antiinterleukin- 6 receptor antibody suppressed angiogenesis and inhibited tumour-stroma interaction. Br J Cancer. 2014;110:469-478.
- Baxter EJ, Scott LM, Campbell PJ, et al. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet. 2005; 365:1054-1061.
- Verstovsek S, Mesa RA, Gotlib J, et al. A double-blind, placebo-controlled trial of ruxolitinib for myelofibrosis. N Engl J Med. 2012;366:799-807.
- Mullighan CG, Zhang J, Harvey RC, et al. JAK mutations in high-risk childhood acute lymphoblastic leukemia. Proc Natl Acad Sci U S A. 2009; 106:9414-9418.
- Xiang Z, Zhao Y, Mitaksov V, et al. Identification of somatic JAK1 mutations in patients with acute myeloid leukemia. Blood. 2008;111:4809-4812.
- Flex E, Petrangeli V, Stella L, et al. Somatically acquired JAK1 mutations in adult acute lymphoblastic leukemia. J Exp Med. 2008; 205:751-758.
- Pikman Y, Lee BH, Mercher T, et al. MPLW515L is a novel somatic activating mutation in myelofibrosis with myeloid metaplasia. PLoS Med. 2006;3:e270.
- Russell LJ, Capasso M, Vater I, et al. Deregulated expression of cytokine receptor gene, CRLF2, is involved in lymphoid transformation in B-cell precursor acute lymphoblastic leukemia. Blood. 2009;114:2688-2698.
- Koskela HL, Eldfors S, Ellonen P, et al. Somatic STAT3 mutations in large granular lymphocytic leukemia. N Engl J Med. 2012; 366:1905-1913.
- Dawson MA, Bannister AJ, Gottgens B, et al. JAK2 phosphorylates histone H3Y41 and excludes HP1alpha from chromatin. Nature. 2009;461:819-822.
- Rui L, Emre NC, Kruhlak MJ, et al. Cooperative epigenetic modulation by cancer amplicon genes. Cancer Cell. 2010;18:590-605.
- Lowenfels AB, Maisonneuve P, Cavallini G, et al. Pancreatitis and the risk of pancreatic cancer. International Pancreatitis Study Group. N Engl J Med. 1993;328:1433-1437.
- Lowenfels AB, Maisonneuve P, DiMagno EP, et al. Hereditary pancreatitis and the risk of pancreatic cancer. International Hereditary Pancreatitis Study Group. J Natl Cancer Inst. 1997;89:442-446.
- Guerra C, Schuhmacher AJ, Canamero M, et al. Chronic pancreatitis is essential for induction of pancreatic ductal adenocarcinoma by K-Ras oncogenes in adult mice. Cancer Cell. 2007;11:291-302.
- Bunt SK, Yang L, Sinha P, et al. Reduced inflammation in the tumor microenvironment delays the accumulation of myeloid-derived suppressor cells and limits tumor progression. Cancer Res. 2007;67:10019-10026.
- Denley SM, Jamieson NB, McCall P, et al. Activation of the IL-6R/Jak/stat pathway is associated with a poor outcome in resected pancreatic ductal adenocarcinoma. J Gastrointest Surg. 2013;17:887-898.
- Nixon AB, Pang H, Starr MD, et al. Prognostic and predictive blood-based biomarkers in patients with advanced pancreatic cancer: results from CALGB80303 (Alliance). Clin Cancer Res. 2013;19:6957-6966.
- Mills LD, Zhang Y, Marler RJ, et al. Loss of the transcription factor GLI1 identifies a signaling network in the tumor microenvironment mediating KRAS oncogene-induced transformation. J Biol Chem. 2013;288:11786-11794.
- Fearon K, Arends J, Baracos V: Understanding the mechanisms and treatment options in cancer cachexia. Nat Rev Clin Oncol. 2013;10:90-99.
- Kocher HM, Mears L, Lea NC, et al. JAK V617F missense mutation is absent in pancreatic cancer. Gut. 2007;56:1174-1175.
- Teague A, Tan B., Lockhart, A. et al. Next-generation sequencing in pancreatic cancer: Revealing genomic mutations beyond KRAS. J Clin Oncol. 2014 (suppl 3, abstr 2008).
- Cerami E, Gao J, Dogrusoz U, et al. The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012;2:401-404.
- Lili LN, Matyunina LV, Walker LD, et al. Evidence for the importance of personalized molecular profiling in pancreatic cancer. Pancreas. 2014;43:198-211.
- Corcoran RB, Contino G, Deshpande V, et al. STAT3 plays a critical role in KRAS-induced pancreatic tumorigenesis. Cancer Res. 2011;71:5020-5029.
- US National Library of Medicine. ClinicalTrials.gov [online], https://clinicaltrials. gov/ct2/show/NCT02117479 (2014).
- US National Library of Medicine. ClinicalTrials.gov [online], https://clinicaltrials. gov/ct2/show/NCT02119663 (2014).
- US National Library of Medicine. ClinicalTrials.gov [online], https://clinicaltrials. gov/ct2/show/NCT01822756.
- US National Library of Medicine. ClinicalTrials.gov [online], https://clinicaltrials. gov/ct2/show/NCT02101021 (2015).
- US National Library of Medicine. ClinicalTrials.gov [online], https://clinicaltrials. gov/ct2/show/NCT01858883, 2015.
- Tolcher AW, Bendell JC, Papadopoulos KP, et al. A phase IB trial of the oral MEK inhibitor trametinib (GSK1120212) in combination with everolimus in patients with advanced solid tumors. Ann Oncol. 2015;26:58-64.
- Yap TA: Challenges in combining novel molecularly targeted agents in cancer medicine. Ann Oncol. 2015;26:9-11.
- Long GV, Stroyakovskiy D, Gogas H, et al. Combined BRAF and MEK inhibition versus BRAF inhibition alone in melanoma. N Engl J Med. 2014; 371:1877-1888.
- Larkin J, Ascierto PA, Dreno B, et al. Combined vemurafenib and cobimetinib in BRAF-mutated melanoma. N Engl J Med. 2014;371:1867-1876.
- Wang-Gillam A, Nywening TM, Sandford DE, et al. Phase IB study of FOLFIRINOX plus PF-04136309 in patients with borderline resectable and locally advanced pancreatic adenocarcinoma. J Clin Oncol. 2015; 33suppl 3; abstr 338).