Publication
Article
Administrative Payment Tasks Could Be Causing Detrimental Effect of Treatment Delays and Nonadherence for Patients With Cancer
Author(s):
A possible cause of some of the cost-related delays and nonadherence to treatment that patients with cancer and cancer survivors experience could be the time and effort they are forced to spend on administrative payment tasks related to their care.
Meredith Doherty, PhD, LCSW

Patients with cancer and cancer survivors frequently have difficulty adhering to the rigorous demands of their treatment for a variety of reasons, and a difficult-to-navigate US health care delivery and finance system is troublesome for providers and patients alike. A possible cause of some of the cost-related delays and nonadherence to treatment that patients and survivors experience could be the time and effort they are forced to spend on administrative payment tasks related to their care, according to findings from a study published in Cancer Epidemiology, Biomarkers & Prevention.
Data from the study showed that patients who reported engaging in more administrative tasks had higher log odds of delaying or forgoing care (b = 0.18; 95% CI, 0.12-0.24) after study authors accounted for age, race/ethnicity, education, and out-of-pocket costs. Additionally, cost-related delays and nonadherence to care were raised by 32% for each unit of increase in administrative payment burden (b = 0.32; 95% CI, 0.18-0.46). Overall, investigators determined that administrative patient burden increased the odds of cost-related delays and nonadherence by 49%.
The study was a secondary analysis of cross-sectional survey data collected by CancerCare, a national nonprofit organization that aims to provide psychological support to patients with cancer. “There was a particular [portion of the CancerCare] survey that focused on financial and insurance concerns of people with cancer,” Meredith Doherty, PhD, LCSW, assistant professor in the School of Social Policy & Practice at the University of Pennsylvania in Philadelphia, said in an interview with OncologyLive. “There were these questions about administrative burdens and questions about cost-related nonadherence. I thought that these things are probably related given what I know about the concepts of administrative burden, nonadherence, and cost-related nonadherence. This was the impetus to start to explore the data in that way.”
To conduct their study, Doherty and her colleagues analyzed survey item responses from a total of 510 US-based patients with cancer and cancer survivors. To be eligible for the study, participants needed to have a history of any cancer besides nonmelanoma skin cancers, have health insurance coverage, and be 25 years or older. The original CancerCare survey contained items regarding demographic characteristics, gross household income, cancer type and status, treatments received, health insurance type, and estimated monthly out-of-pocket expenses related to their care.
Investigators identified 10 items of interest to include in their data set: 5 related to administrative tasks and 5 connected to cost-related nonadherence. The items deemed to be related to administrative payment tasks asked patients how often they did the following: received an estimated cost before agreeing to a treatment their doctor recommended, appealed the denial of benefits from their insurance company, found out the out-of-pocket cost before filling a prescription for a treatment drug, asked the insurance company for help in understanding coverage, and/or found out the out-of-pocket cost before getting laboratory tests or scans. The 5 items investigators identified as being pertinent to cost-related delays and nonadherence asked patients how often they did the following to reduce their expenses related to cancer treatment: delayed or skipped appointments, delayed or skipped blood work, delayed or skipped follow-up blood testing, cut pills in half, and/or skipped dosages of prescribed drugs (Table).
Table. Patient Answers to Items Regarding Administrative Payment Tasks Cost-Related Delays, and Care Nonadherence in CancerCare Survey
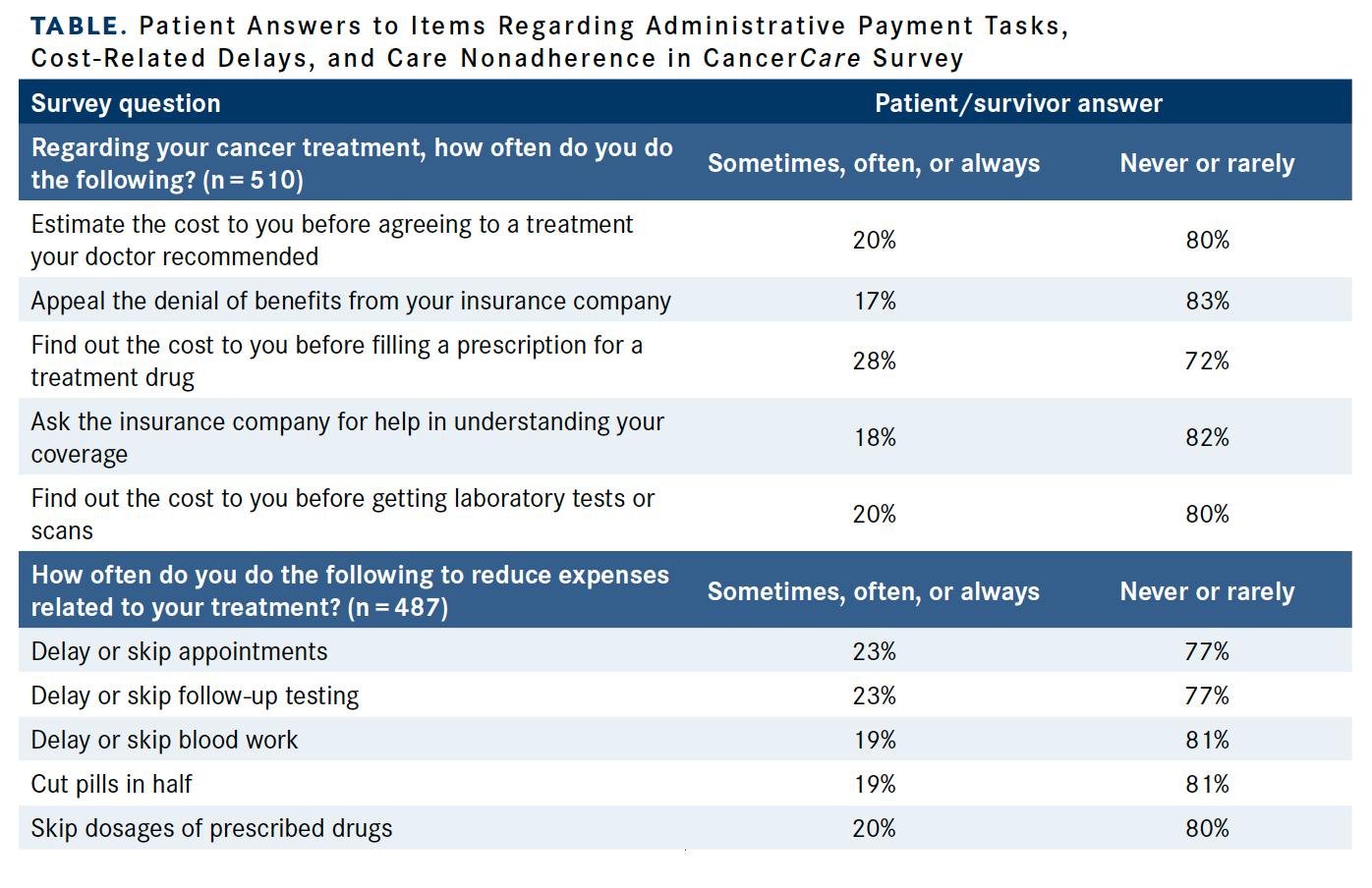
Patients’ responses to each of the 10 survey items were assigned values of 0 (never), 1 (rarely), 2 (sometimes), 3 (often), and 4 (always). These findings were compiled into 2 additive scales for each set of questions with scores ranging from 0 to 20, with higher scores representing greater cost-related nonadherence and administrative burden.
Study authors analyzed the data using 2-part modeling to predict cost-related delays and treatment nonadherence. The models first used a logit function to estimate the likelihood of a nonzero outcome, and then generalized linear modeling was used to estimate the relationship between the predictor variables of administrative burden and other covariates and cost-related delays and nonadherence. Investigators also used univariate 2-part models to estimate the correlations between predictor variable and cost-related delays and nonadherence; this information was retained for the multivariate model if the variables displayed a P value of less than .01.
Most respondents who completed the survey and were included in the cross-sectional analysis were women (65%), older than 55 years (58%), and White (71%). The most commonly reported household income range was $50,000 to $74,999 (21%), and less than half of the population had attained an education level of a bachelor’s degree or higher (48%). Insurance types consisted of Medicare/Medicaid (55.1%), employer sponsored (36.9%), Medicare plus Medigap (10.5%), marketplace (9.3%), other (5.2%), and Tricare/CHAMPUS (2.7%).
The most common cancer types included in the sample were early-stage breast (22.3%), prostate (10.2%), and colorectal (8%). The sample also included patients with bladder (3.5%), brain (2.2%), metastatic breast (6.5%), gynecologic (6.7%), head and neck (1.8%), kidney (4.9%), leukemia (4.7%), liver (0.4%), lung (5.3%), lymphoma (3.7%), melanoma (2.4%), myeloma (0.8%), pancreatic (2.4%), stomach (0.6%), thyroid (4.9%), and other (8.8%) cancers.
“There’s a huge amount of heterogeneity in the cancer types, the incomes, the regions in which people live, and the states in which people live,” Doherty said. “All those [factors are correlated] to variation in the way that health care is delivered and the quality of care. If we dug deeper and looked at administrative burdens in a very specific population, we might be able to see a lot more. In some cases, heterogeneity in your sample gives you a lot of strength. In this case, I’d say we maximized it to understand differences between groups.”
Fifty-five percent of patients answered the survey by indicating that they never or rarely engaged in any of the tasks that were inquired about. Only 9% of respondents said they engaged in at least 4 administrative payment tasks, and the mean total tasks was 1 (SD, 1.43) of a possible 5. At the item level, each of the 5 administrative payment tasks was associated with cost-related delays and/or nonadherence.
Notably, additional findings from the study showed 2 groups of older patients, defined as those aged 55 to 64 years (b = –1.26; 95% CI, –2.21 to –0.31) and those aged 65 to 74 years (b = –1.77; 95% CI, –2.75 to –0.80), both experienced lessened log odds of engaging in cost-related nonadherence to care compared with younger patients aged 25 to 34 years. Moreover, findings from an adjusted generalized linear model revealed that patients aged 55 to 64 years displayed an association with reduced cost-related nonadherence (b = –3.02; 95% CI, –4.99 to –1.06).
There were also disparities reported in terms of cost-related nonadherence among other patient subgroups. Black patients displayed increased log odds of reporting cost-related nonadherence (b = 1.10; 95% CI, 0.33-1.87) compared with White patients; however, it was not significantly associated with cost-related nonadherence according to findings from the generalized linear model. Patients who said that their monthly out-of-pocket medical costs exceeded $500 had greater log odds of reporting cost-related nonadherence compared with those who reported monthly costs of less than $100 (b = 1.17; 95% CI, 0.40-1.95). This finding was again observed when investigators used the generalized linear model (b = 2.69; 95% CI, 0.70-4.69).
“All the labor and effort that it takes to resolve payment issues to make sure that you’re adequately informed in order to make decisions about payment or dispute payment issues [is something that] many of us are unfortunately familiar with,” Doherty said. “We’ve all tried to seek clarification on a bill related to health care; [things like] that were correlated with this nonadherence. The implications and what we can hypothesize about, what the mechanisms are underlying that, are interesting to think about.”
Regarding these potential mechanisms causing the relationship between payment administrative tasks and care nonadherence and cost-related treatment delays, Doherty explained that it’s hard to pin down a specific cause because of the multifactional nature of the issue, both in patient subgroups and in general. Based on her knowledge of literature in the area, she hypothesized that structural vulnerabilities often divided along race and class lines, such as level of access to health care, lack of knowledge regarding how to deal with the health care system, and lack of access to personalized resources to understand their disease, could all potentially play a role in the disparities between patient subgroups that were observed.
In terms of study limitations, Doherty noted that the study was exploratory in nature with the effect of simply establishing that there is a relationship between administrative burden and cost-related treatment delays and nonadherence. The data provide a correlational but not a causal link between the 2 variables. She also explained that the survey was administered online, and some patients/survivors received a diagnosis of cancer more than 4 years ago. However, Doherty said that study authors measured for recall bias and found that time since cancer diagnosis and treatment did not have a significant effect on the findings.
Reference
Doherty M, Thom B, Gardner DS. Administrative burden associated with cost-related delays in care in U.S. cancer patients. Cancer Epidemiol Biomarkers Prev. Published online August 30, 2023. doi:10.1158/1055-9965.EPI-23-0119