Borgen Shares the Latest on Upcoming Virtual Meetings, COVID-19, and Breast Cancer Treatment
Patrick I. Borgen, MD, highlights the effects of the coronavirus disease 2019 (COVID-19) pandemic on the field of oncology.
The effects of the coronavirus disease 2019 (COVID-19) pandemic have reverberated across the field of oncology, said Patrick I. Borgen, MD, especially with regard to major medical meetings, which are expected to remain virtual for the foreseeable future.
At the Maimonides Medical Center in Brooklyn, New York, where Borgen serves as the chair of the Department of Surgery, the COVID-19 pandemic caused a complete cessation of elective surgeries for patients with breast cancer, as well as significant changes and delays to treatment.
Now, months into the outbreak, Borgen says that the center is “back to business as usual” and that patient outcomes do not appear to have been negatively impacted by the effects of COVID-19.
However, not all aspects of the field have returned to normal. For example, upcoming medical meetings, such as the 8th Annual Giants of Cancer Care® Awards Ceremony, the 38th Annual Chemotherapy Foundation Symposium (CFS), the San Antonio Breast Cancer Symposium (SABCS) 2020 Virtual Meeting, and the 38th Annual Miami Breast Cancer Conference will be hosted virtually.
Despite COVID-19, the field of breast cancer continues to evolve, explained Borgen, who cited recent regulatory approvals and the growing role of immunotherapy as prime examples of the pace at which progress has been made.
In an interview with OncLive®, Borgen, who is also head of the Maimonides Breast Center at Maimonides Cancer Center, provided insight into upcoming virtual medical meetings, the lasting effects of the COVID-19 pandemic on the treatment of patients at Maimonides Medical Center, and key data that have emerged in the breast cancer space.
OncLive®: We are going to be celebrating the 8th Annual Giants of Cancer Care® Awards Ceremony in November 2020. What can you tell us about this year’s inductees and the impact they have had on the treatment of patients with cancer?
Borgen: Giants of Cancer Care® is a virtual Hall of Fame for oncologists and cancer researchers. With our new class of inductees, we are again shining a spotlight on some of the brightest minds and some of the shoulders that we stand on today as we work in the cancer field.
In particular, my former partner, Clifford A. Hudis, MD, [of Memorial Sloan Kettering Cancer Center (MSKCC)], who was the chief of breast medical oncology at MSKCC when I was chief of breast surgery [will be inducted]. Cliff and I ran that division for 12 or 15 years. Having worked with Cliff every day, and seeing his contributions, work ethic, and passion to eliminate breast cancer, I am incredibly proud to be giving him his Giants of Cancer Care® award this year.
The 38th Annual CFS will also take place in a virtual format this November. What insight can you provide into the upcoming meeting?
The CSF [meeting] is virtual, of course. For an event that is held in Times Square usually, [moving to a virtual platform] is very important. New Yorkers have been very disciplined in their approach to COVID-19 and in their willingness to wear masks and socially distance. Of course, all of our meetings in New York will be virtual for the foreseeable future. We have a session that I am excited about at this year’s CFS regarding where we are now with COVID-19 and cancer. I will be moderating the panel that will be looking at this.
I am looking forward to CFS this year, and I am particularly looking forward to the Giants of Cancer Care® awards ceremony and our COVID-19 panel.
In March 2021, the 38th Annual Miami Breast Cancer Conference will take place, but on a virtual interactive platform. What are some of the benefits and drawbacks to moving the meeting to a virtual setting?
We are disappointed that we won’t be face-to-face at the beautiful Fontainebleau hotel in Miami, Florida this year, but we are also excited about our chance to expand the footprint of the Miami Breast Cancer Conference. We can add speakers, parallel sessions, and topics that we didn’t cover before. If you think about the live [conference], which took place from Thursday afternoon to Sunday morning, we had about 80 to 85 lectures. In the virtual space, we can have 185 lectures. We can have deep dive breakout sessions, [meaning] whole sessions dedicated to opioid elimination, oncoplastic surgery, and HER2-targeted therapies. Although we are disappointed that we won’t be seeing each other in person, we are really excited about this new platform.
Now that we are several months into the COVID-19 pandemic, how has the disease affected the care of patients with cancer at Maimonides Medical Center?
Our zip code in southern Brooklyn was the tip of the spear of the COVID-19 surge, certainly on the East Coast. If we look at the zip codes [that had the largest number of] COVID-19 hospitalizations, we had 3 of the top 7 in our area. We wound up treating over 6000 patients for COVID-19, admitted several thousand, and of course, had hundreds of patients die from COVID-19.
All [elective] surgery [was] stopped by state law. Interventional cardiology and orthopedic surgery [were also halted] during the peak, partly because our recovery rooms were converted into intensive care units [ICUs].
At the peak of the COVID-19 pandemic, we had 380 patients on ventilators, just in our hospital. We did our best to see patients virtually and to treat breast cancer as aggressively as we could while we waited for surgeries [to resume].
Now, we are seeing that [that approach] worked; we are seeing that those patients did not pay a heavy price for that delay [in treatment]. We are experiencing a small peak now. We have 30 patients in the hospital, but we are not anticipating a strong surge [of COVID-19 cases].
We have isolated our COVID-19 patients in a way that we were not able to in March, April, and May 2020. Our operating rooms and our ICUs are really COVID-19 free. Therefore, we are back to business as usual at Maimonides Medical Center.
Have any data been recently published regarding the effects of COVID-19 on the care of patients with cancer?
A very important paper was published [recently] in the Lancet, which looked at over 1000 patients across 235 hospitals. These were patients who had surgery and tested positive for COVID-19 7 days before surgery or up to 30 days after surgery. The results were quite alarming. The rate of major pulmonary complications was over 50%; in cardiac surgery, the rate was 90%.
We have to carefully continue to raise our threshold for who has surgery and when. We know that there is a hypercoagulable state that comes with COVID-19, which makes all operations for breast cancer, colon cancer, and brain cancer, [for example], really difficult.
The 2020 ESMO Virtual Congress took place in September. What key data in breast cancer would you like to highlight?
It is really exciting to look at what happened at the 2019 SABCS and the 2020 ASCO Virtual Scientific Program. ESMO capped [these meetings]. Now, we have 2 or 3 layers of depth in HER2-targeted therapy. Five drugs were approved this year; that is unprecedented. I remember early in my career when 1 or 2 drugs were approved over the course of 5 years. Particularly in the HER2-positive space, we now have so many [agents] for first-line therapy, as well as second- and third-line therapies. More [agents] are coming.
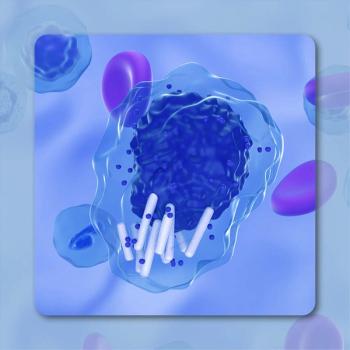
We have learned a lot about CDK4/6 inhibitors and T-cell modulators. We are poised to move immuno-oncology into the adjuvant space in breast cancer. Last year during the 2019 Miami Breast Cancer Conference, we learned that atezolizumab [Tecentriq], a PD-1/PD-L1 inhibitor was approved in metastatic triple-negative breast cancer [TNBC]. Now, we are waiting for the approval of pembrolizumab [Keytruda] in the adjuvant space. Immuno-oncology is real, and it is here to stay.
Is nab-paclitaxel the only taxane that can be used in combination with atezolizumab in metastatic TNBC?
The original atezolizumab study in stage IV TNBC used nab-paclitaxel [Abraxane]. Nab-paclitaxel is a great drug, but it had been put on the shelf mostly. Therefore, we are trying to get clarity on whether we could use a different taxane. Could we use paclitaxel along with the PD-1/PD-L1 inhibitor? That picture is getting a little bit clearer.
What other questions need to be answered regarding the role of immunotherapy in breast cancer?
How we sequence therapies is a very different [topic]. It used to be that we gave concurrent cytotoxic chemotherapies. CMF [cyclophosphamide, methotrexate and fluorouracil] was our first [choice of chemotherapy], then AC [doxorubicin hydrochloride and cyclophosphamide], and then AC followed by T [paclitaxel]. Chemotherapy doublets or triplets were almost always [available]. What we are imagining now is very different, and that is a sequence of second-, third-, and fourth-line therapies.



































