Overview of Relapsed/Refractory Diffuse Large B-Cell Lymphoma
Episodes in this series
Matthew J. Frigault, MD: Prior to CAR [chimeric antigen receptor] T cells, we classified diseases into 2 main categories in the relapse or up-front refractory setting: chemotherapy refractory and chemotherapy sensitive. The distinction here is trying to determine who will gain benefit from addition of an autologous stem cell transplant using high-dose chemotherapy preconditioning. Typically, when patients relapsed following first-line therapy, depending whether it was within a certain time period of 12 months or so, we would classify these patients as high risk, chemotherapy refractory, or chemotherapy sensitive. Based on that distinction, we proceed forward to salvage chemotherapy, typically in the second line, with the hopes that we’ll get an adequate response to then bring these patients on high-dose chemotherapy and stem cell rescue or an autotransplantation.
We know that patients who had at least a partial response or more—ideally a complete response—to salvage therapy would then have a relatively high success rate with autologous stem cell transplant and high-dose chemotherapy. The premise is that high-dose chemotherapy for chemotherapy-sensitive disease would impart a survival benefit. However, we’ve seen over time that the degree of partial response does matter, and any residual disease following salvage therapy may be concerning. Those patients do have higher rates of relapse, as opposed to those who have a complete response following cycle 2 of salvage therapy.
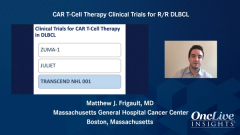
It is typically recommended that patients are assessed, and if they do have an adequate response, they proceed to autologous stem cell transplant. However, we’re seeing the field evolve. For patients who do not achieve an adequate, complete response, may be in a partial response, or are considered high risk, we sometimes consider consolidation with CAR T cells as defined by calling that chemotherapy-refractory disease. This is constantly evolving. There are multiple clinical trials that are underway. They are looking at randomized phase 3 studies of all 3 major products—tisagenlecleucel, lisocabtagene maraleucel, and axicabtagene ciloleucel—comparing autologous stem cell transplant following salvage chemotherapy with up-front CAR T cells.
They are looking to see which approach has overall survival and progression-free survival benefits. This is a very evolving field. The goal at this point in time is to attempt salvage chemotherapy and proceed forward with autologous stem cell transplant if appropriate. If a patient were to relapse, the options then include things like CAR T cells, recently approved polatuzumab, or recently approved CD19 antibody MOR208.
From my standpoint, when we’re looking at patients following salvage chemotherapy, our goal is to find that truly chemotherapy-sensitive population. The field, at least at our institution, is moving forward or moving toward complete responses going on to autologous stem cell transplant. However, any partial response is going directly to CAR T cells. This is mainly based on the fact that historical data have shown us that partial responses do have inferior outcomes and CAR T cells do allow for ongoing benefit. This includes other abstracts and papers that were published in the past few years looking at retrospective analysis of JULIET. Patients who had CAR T-cell consolidation following third-line salvage therapy without measurable disease had benefit from CAR T-cell therapy. That was published in Blood Advances by Michael Bishop.
That is our practice. As we look at patients who are candidates for CAR T cells, it’s not so much who is a candidate for CAR T cell therapy, but how do you optimize the patient for CAR T cells? Later, we’ll get into the ideal patient population. They are older patients, patients we may not consider to be transplant eligible. That is defined by being older age, having lower ECOG performance scores, and being higher risk for comorbidities. However, we have successfully been able to treat patients well into their 80s, patients with cardiac disease, and patients with renal dysfunction.
It’s all patient optimization, and early and up-front discussion with the patient, as well as some co-consultants, to come up with an appropriate strategy for bringing the patient forward to CAR T-cell therapy, given that these are lifesaving therapies. You can expect upward of 40% to have progression-free survival with all 3 of these products going out 12 to 24 months. These fundamentally changed how we treat patients. We’re saving lives. There are obviously competing risks, but appropriate optimization can usually get a patient safely through CAR T-cell therapy.
Transcript Edited for Clarity