Myeloproliferative Neoplasms
Latest News
Latest Videos

CME Content
More News

Sikander Ailawadhi, MD, discusses characteristics of myelofibrosis that influence decisions between JAK inhibitors, highlights differences between bispecific antibodies to consider when managing diffuse large B-cell lymphoma, and more.

David A. Sallman, MD, discusses the rationale for conducting a phase 2, multi-institutional, investigator-initiated clinical trial on the use of fedratinib in patients with myelodysplastic syndromes/myeloproliferative neoplasm overlap syndromes and chronic neutrophilic leukemia.

Experts explain how polycythemia vera is diagnosed and the typical symptoms a patient may present with.

The oral selective PIM1 kinase inhibitor TP-3654 appeared to be well tolerated and to show early signals of spleen volume reduction, symptom improvement, and correlating cytokine reductions in patients with relapsed or refractory myelofibrosis, according to preliminary data.
The presence of mutated SRSF2 in knock-in mouse models of JAK2 V617F–driven myeloproliferative neoplasms reduced the rate of polycythemia and hampered hematopoietic progenitor functions.

OncLive® will be LIVE with OncLive® News Network: On Location at the 2023 ASH Annual Meeting. Each day, we will broadcast a series of interviews with top thought leaders, to learn their thoughts and reactions to data presented across oncology during the conference.

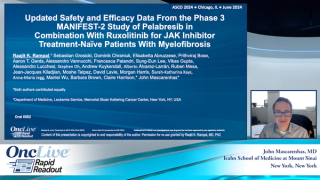
Raajit K. Rampal, MD, PhD, discusses findings from the phase 3 MANIFEST-2 trial investigating pelabresib in combination with ruxolitinib for JAK inhibitor–naive patients with myelofibrosis.

Pelabresib plus ruxolitinib demonstrated a 35% or greater reduction in spleen volume and trended toward reducing mean absolute total symptom score (TSS) as well as improving TSS reduction by 50% at 24 weeks in patients with JAK inhibitor–naive myelofibrosis.
Oral decitabine/cedazuridine and parenteral hypomethylating agents were associated with similar levels of comorbidities and disease burden in patients with myelodysplastic syndrome.

Up-front treatment with navitoclax plus ruxolitinib significantly reduced spleen volume by 35% or more at week 24 vs ruxolitinib plus placebo in patients with myelofibrosis; however, a significant difference was not observed in total symptom score v. 4.0 between the arms, according to data from the phase 3 TRANSFORM-1 study.

The high-precision cell therapy Orca-T demonstrated high rates of relapse-free survival, overall survival, and graft-vs-host disease RFS at 1 year, as well as a low incidence of GVHD in patients with intermediate- to high-risk myelodysplastic syndrome.
A machine learning, artificial intelligence algorithm analyzing diagnostic bone marrow biopsy digital whole-slide images was able to effectively differentiate with 92.3% accuracy between prefibrotic primary myelofibrosis and essential thrombocythemia.

Amer Zeidan, MBBS, discusses classification and treatment updates for patients with myelodysplastic syndrome.

Marina Kremyanskaya, MD, PhD, discusses disease and patient characteristics that influence the choice between hydroxyurea and interferon therapy for patients with polycythemia vera or essential thrombocythemia.

Treatment with the combination of pelabresib and ruxolitinib led to a statistically significant and clinically meaningful improvement in spleen volume reduction vs placebo plus ruxolitinib in patients with JAK inhibitor-naive myelofibrosis, meeting the primary end point of the phase 3 MANIFEST-2 trial.

Dr DiNardo discusses the the FDA approval of ivosidenib for patients with relapsed/refractory IDH1-mutant myelodysplastic syndromes, the unique mechanism of action of ivosidenib, and key efficacy and safety findings from the AG120-C-001 trial.
Patients with myelodysplastic syndrome harboring a TP53 mutation experienced a survival benefit with allogeneic hematopoietic cell transplantation compared with non-HCT treatment regardless of TP53 allelic status.

Gaby Hobbs, MD, discusses how research into the biology of myelofibrosis has propelled the development of novel therapies for this patient population and highlights the role that biomarkers play in the diagnosis, prognosis, and treatment response evaluation for these patients.
The European Medicines Agency’s Committee for Medicinal Products for Human Use has adopted a positive opinion supporting the approval of momelotinib for the treatment of disease-related splenomegaly or symptoms in adult patients with moderate to severe anemia with primary myelofibrosis, post–polycythemia vera myelofibrosis, or post–essential thrombocytopenia myelofibrosis who have not been exposed to a JAK inhibitor or who had received prior ruxolitinib.

Douglas A. Tremblay, MD, discusses the prevalence of myelodysplastic syndrome/myeloproliferative neoplasm overlap syndromes and the evolving treatment paradigm for these diseases.

Andrew T. Kuykendall, MD, discusses the importance of the approval of momelotinib in the treatment of patients with anemic symptomatic myelofibrosis, key efficacy and safety data from the MOMENTUM trial that supported the decision, and unanswered questions regarding the agent’s potential role in other subsets within this population.

Anthony M. Hunter, MD, discusses the evolution of JAK inhibitors in myelofibrosis, a topic that was highlighted in a presentation at the 2023 SOHO Annual Meeting.

Courtney D. DiNardo, MD, MSCE, discusses the significance of the FDA approval of ivosidenib in patients with relapsed/refractory, IDH1-mutated myelodysplastic syndromes.

The FDA has approved ivosidenib (Tibsovo) for the treatment of adult patients with relapsed/refractory myelodysplastic syndromes with a susceptible IDH1 mutation, as detected by an FDA-approved test.

Andrew Kuykendall, MD, discusses frontline cytoreductive treatment options for patients with polycythemia vera.