
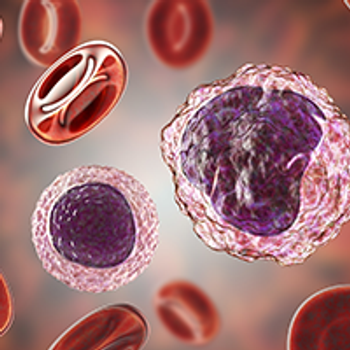
The FDA has granted fast track designation to IDP-023 for the treatment of patients with non-Hodgkin lymphoma and multiple myeloma

Your AI-Trained Oncology Knowledge Connection!


The FDA has granted fast track designation to IDP-023 for the treatment of patients with non-Hodgkin lymphoma and multiple myeloma

The European Medicines Agency has validated a marketing authorization application seeking the approval of nirogacestat for patients with desmoid tumors.

The blood cancer expert comes to Sylvester Comprehensive Cancer Center after leading the discovery and testing of several immunotherapy approaches.

In case you missed it, below is a recap of all drugs that have been approved by the FDA in February 2024.

The FDA has approved a label expansion for ibrutinib with an oral suspension formulation in all current indications.

Nikhil A. Gopal, MD, discusses the benefit of belzutifan in addition to effective immunotherapy-based regimens in advanced RCC.

Pasi A. Jänne, MD, PhD discusses the FDA approval of osimertinib plus chemotherapy for patients with EGFR-positive non–small cell lung cancer.

The FDA granted an orphan drug designation to LUT014 for the treatment of EGFR inhibitor–induced acneiform rash.

Northwestern Medicine scientists have discovered the Achilles heel of chemotherapy-resistant ovarian cancer—its hunger for cholesterol.

The National Comprehensive Cancer Network recommends ropeginterferon alfa-2b as first-line cytoreductive therapy for polycythemia vera.

Andre H. Goy, MD, discusses how the ZUMA-18 trial data support the benefit of earlier-line use of brexucabtagene autoleucel in mantle cell lymphoma.

The FDA granted fast track designation to 9MW2821 for potential use in advanced, recurrent, or metastatic esophageal squamous cell carcinoma.

Rusfertide displayed activity in phlebotomy-dependent polycythemia vera.

Bezuclastinib plus BSC improved mast cell burden and total symptom score vs placebo plus BSC in adult patients with nonadvanced systemic mastocytosis.

The FDA has granted breakthrough therapy designation to NVL-520 for pretreated, metastatic ROS1-positive non–small cell lung cancer.

The biologics license application for first-line tislelizumab plus chemotherapy for gastric/gastroesophageal junction cancer has been accepted by the FDA.

The FDA has granted priority review to the sBLA of epcoritamab for relapsed/refractory follicular lymphoma.

Three Virginia health systems together will serve as one of eight groups in the U.S. to conduct research for the Cancer Screening Research Network.

Patients with mismatch repair–deficient, immunohistochemistry-intact colorectal cancer or endometrial cancer benefit from immune checkpoint inhibitors.
Daniel Olson, MD, discusses the significance of the FDA approval of lifileucel for patients with advanced melanoma.

Riccardo Lencioni, MD, discusses how TACE, durvalumab, and bevacizumab, could represent a new standard of care in embolization-eligible HCC.

Manish A. Shah, MD, discusses 5-year outcomes from phase 3 KEYNOTE-590 study of first-line pembrolizumab plus chemotherapy for advanced esophageal cancer.

In case you missed it, read a recap of every episode of OncLive On Air recorded in January 2024.

McKesson has received approval from the CMS to participate in the Merit-based Incentive Payment System as a Qualified Clinical Data Registry.

The European Medicines Agency’s CHMP has recommended the approval of tislelizumab in the first- and second-line for non–small cell lung cancer.

BAY 2927088 has received breakthrough therapy designation by the FDA for pretreated non–small cell lung cancer harboring activating HER2 mutations.

Benjamin Philip Levy, MD, details how antibody-drug conjugates are shifting the HER2-mutated non–small cell lung cancer treatment paradigm.
Jacob Shreve, MD, MS, highlights the intersection between artificial intelligence and personalized medicine, as well as its potential utility in gastrointestinal cancers.
Real-world ruxolitinib use in chronic GVHD was primarily in the second- or third-line, lasted for a median of 8 months, and involved dose adjustments.

Encouraging data with RFS, OS, and NRM for Orca-T was also matched in a population of patients with hematologic cancers aged 55 years and older.