Haploidentical donor transplantation led to stronger anti-leukemia activity compared with matched sibling donor transplantation in transplant-eligible patients with minimal residual disease–positive acute lymphoblastic leukemia.

Your AI-Trained Oncology Knowledge Connection!

Haploidentical donor transplantation led to stronger anti-leukemia activity compared with matched sibling donor transplantation in transplant-eligible patients with minimal residual disease–positive acute lymphoblastic leukemia.
Basiliximab proved to be an effective second-line treatment option for pediatric patients with steroid-refractory acute graft-versus-host disease that developed following haploidentical hematopoietic stem cell transplantation.
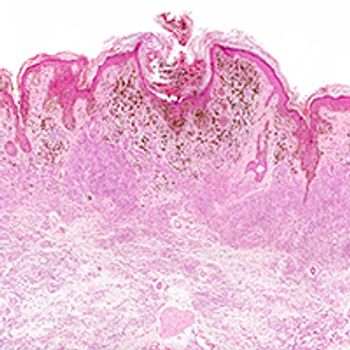
Patients with unresectable or metastatic melanoma showed durable responses following treatment with the novel PD-1 inhibitor prolgolimab.

Two analyses presented at the 2019 ESMO Immuno-Oncology Congress provided data supporting pembrolizumab, either as monotherapy or in combination with chemotherapy, as a first-line treatment option in patients with nonsquamous non–small cell lung cancer, regardless of KRAS mutational status.

Few immune-mediated adverse events were observed with frontline durvalumab plus platinum-based therapy and etoposide in patients with extensive-stage small cell lung cancer, and no treatment-emergent antidrug antibodies were elicited by the PD-L1 inhibitor, according to an analysis of the phase III CASPIAN trial reported at the 2019 ESMO Immuno-Oncology Congress.

First-line treatment with nivolumab combined with low-dose ipilimumab was safe and showed encouraging overall survival, regardless of PD-L1 expression, in patients with advanced non–small cell lung cancer, including those with comorbidities or poor ECOG performance status.

A triplet regimen of the CXCR4 antagonist BL-8040 plus pembrolizumab and standard chemotherapy showed promising antitumor activity in the second-line setting for the treatment of patients with metastatic pancreatic ductal adenocarcinoma.

The first-line combination of nivolumab and platinum-based chemotherapy improved overall survival, progression-free survival, and objective response rate compared with chemotherapy in patients with squamous non–small cell lung cancer, but did not improve survival in those with nonsquamous disease.

PD-L1-high status, determined via 3 separate immunohistochemistry assays, and blood tumor mutational burden strongly favored atezolizumab over platinum-based chemotherapy and supports the PD-L1 inhibitor as a first-line treatment option in patients with advanced non–small cell lung cancer.

Patients with high-risk relapsed/refractory chronic lymphocytic leukemia who failed or were intolerant of ibrutinib derived more benefit from CD19‐targeted CAR T-cell therapy when the BTK inhibitor was concurrently administered than when it was not.

Nearly three-fourths of patients with relapsed/refractory primary mediastinal large B-cell lymphoma responded to a combination of nivolumab (Opdivo) plus brentuximab vedotin (Adcetris).

The CAR T-cell therapy lisocabtagene maraleucel demonstrated high rates of response, including minimum residual disease in blood and marrow in patients with relapsed/refractory chronic lymphocytic leukemia or small lymphocytic lymphoma.

Acalabrutinib elicited high rates of response as well as prolonged survival and was well tolerated in patients with chronic lymphocytic leukemia who demonstrated intolerance to ibrutinib.

In a careful evaluation of chemotherapy‐free regimens, the combination of obinutuzumab plus venetoclax compared to obinutuzumab plus chlorambucil, objective and complete response rates, as well as progression-free survival were superior with the venetoclax combination in the overall study population and across all genetic subgroups evaluated in patients with chronic lymphocytic lymphoma.

Patients with activated B-cell-type diffuse large B-cell lymphoma with a poor prognosis may benefit from frontline treatment with lenalidomide plus standard R-CHOP, according to subgroup data from the phase III ROBUST trial presented at the 2019 International Conference on Malignant Lymphoma.

Chemotherapy-free treatment with single-agent acalabrutinib provided a statistically significant and clinically meaningful improvement in progression-free survival compared with physicians’ choice of standard therapy in patients with previously treated chronic lymphocytic leukemia.

Ibrutinib monotherapy significantly improved event- and progression-free survival compared with placebo in treatment-naïve patients with early-stage, asymptomatic chronic lymphocytic leukemia.

Despite promising progression-free survival and response data with venetoclax in combination with bortezomib and dexamethasone, an increased number of deaths due to infection in the experimental arm marred overall survival findings in patients with relapsed/refractory multiple myeloma.

Hu5F9-G4 (5F9), a first-in-class antibody targeting CD47, used as monotherapy or in combination with standard azacitidine was well tolerated and provided deep and durable responses in patients with acute myeloid leukemia or myelodysplastic syndrome, according to findings from a phase IB study presented at the 2019 European Hematology Association Congress.

The combination of rigosertib and azacitidine demonstrated improved response rates over single-agent azacitidine in patients with higher-risk myelodysplastic syndrome, including patients naïve to a hypomethylating (HMA) agent and those who were refractory to HMAs.

Frontline therapy with ibrutinib was successfully administered for more than 60 months in patients with chronic lymphocytic leukemia aged 65 years and older and provided improved progression-free and overall survival compared with chlorambucil.

Imetelstat treatment may allow patients with debilitating anemia due to myelodysplastic syndrome to remain transfusion-free for extended periods of time.

Atezolizumab plus bevacizumab, carboplatin, and paclitaxel has emerged as a potential new standard of care for patients with EGFR-positive metastatic nonsquamous non–small cell lung cancer who have failed prior TKIs.

No overall survival advantage was obtained from maintenance therapy comprising nivolumab (Opdivo) alone or in combination with ipilimumab (Yervoy) over placebo in patients with extensive-stage small cell lung cancer.

Final results from 2 phase I expansion cohorts of frontline osimertinib (Tagrisso) presented at the 2019 European Lung Cancer Congress confirmed the efficacy of the third-generation TKI in patients with EGFR-positive non­–small cell lung cancer.

Patients with ROS1-positive non–small cell lung cancer showed high response rates and durable responses following treatment with entrectinib.

Patient reported outcomes according to PD-L1 expression did not show clinically meaningful differences in quality of life with either durvalumab or placebo in patients with stage III non–small cell lung cancer, according to a retrospective analysis of the phase III PACIFIC study.

The initial overall survival analysis of the phase III MYSTIC trial of first-line durvalumab (Imfinzi) alone or in combination with tremelimumab compared with platinum-based chemotherapy in patients with metastatic non–small cell lung cancer, may have been confounded by high rates of post-study immunotherapy given in the control arm.

Kidney complications often occur following successful hematopoietic stem cell transplantation from a myriad of underlying etiologies.

While complex, criteria for diagnosing transplant-associated thrombotic microangiopathy following hematopoietic stem cell transplantation should be closely followed and should begin with screening.
Published: September 8th 2020 | Updated:
Published: September 9th 2020 | Updated:

Published: October 10th 2016 | Updated:

Published: October 18th 2016 | Updated:

Published: October 20th 2016 | Updated:

Published: October 20th 2016 | Updated: