
Neoadjuvant nivolumab plus ipilimumab demonstrated almost a tripling in objective response rate compared with the PD-1 inhibitor alone but at the cost of significant added grade 3 adverse events for patients with high-risk resectable melanoma.

Your AI-Trained Oncology Knowledge Connection!


Neoadjuvant nivolumab plus ipilimumab demonstrated almost a tripling in objective response rate compared with the PD-1 inhibitor alone but at the cost of significant added grade 3 adverse events for patients with high-risk resectable melanoma.

The combination of the CD122-biased cytokine NKTR-214 and the PD-1 inhibitor nivolumab demonstrated target lesion reductions of 72% for patients with advanced cancers.

The combination of nivolumab and BMS-986205 generated promising response rates without increasing adverse effects in patients with advanced cervical or bladder cancers.

Jason J. Luke, MD, assistant professor of medicine, University of Chicago Medicine, discusses a study evaluating the IDO1 inhibitor BMS-986205 as a monotherapy and in combination with nivolumab in patients with advanced cancers.

Nivolumab demonstrated a 24% overall response rate among patients with a range of non-colorectal cancers with mismatch repair deficiency who were identified through the NCI-MATCH trial.

The high rates of cerebral edema seen with JCAR015 in the phase II ROCKET trial were attributed to early and rapid chimeric antigen receptor (CAR)-modified T-cell expansion and a rise in interleukin-15 levels, a finding that could help inform future CAR T-cell usage.

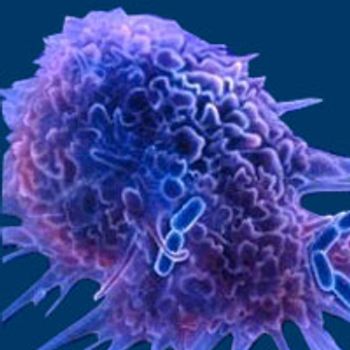
A variety of adoptive T-cell therapy strategies have shown promise in clinical studies with recent FDA approvals granted to CAR-modified T-cell therapies, representing the potential for future combination strategies.
A novel immune checkpoint called PVRIG is currently in development.

Sonja Althammer, PhD, Team Leader Bioinformatics at Definiens, Munich, Bavaria, Germany, discusses a study looking to define a subgroup of patients with non–small cell lung cancer (NSCLC) who respond well to treatment with the PD-L1 inhibitor durvalumab.

Susan Lutgendorf, PhD, professor and Starch Faculty Fellow, Psychological and Brain Sciences, College of Liberal Arts and Sciences, University of Iowa, discusses the impact of lack of support on patients with ovarian cancer. Lutgendorf spoke on this during an interview at the SITC 31st Annual Meeting and Associated Programs.

Lisa Butterfield, PhD, professor of Medicine, Surgery and Immunology, director, University of Pittsburgh Cancer Institute Immunologic Monitoring and Cellular Products Laboratory, University of Pittsburgh, discusses the goals of the Society for Immunotherapy of Cancer (SITC) Immune Biomarkers Task Force during an interview at the SITC 31st Annual Meeting and Associated Programs.

Recent research suggests that the presence of PD-L1–positive and CD8+ cells may be useful for predicting responses in patients with non-small cell lung cancer who have been treated with durvalumab.

The combination of nivolumab and ipilimumab led to a high response rate and improved overall survival versus historical controls for patients with pretreated metastatic urothelial carcinoma.

Pembrolizumab monotherapy reduced the risk of death by 27% compared with chemotherapy for patients with advanced urothelial carcinoma whose disease progressed after prior treatment.

The combination of lirilumab and nivolumab resulted in an objective response rate of 24.1% in patients with squamous cell carcinoma of the head and neck.

Joaquim Bellmunt, MD, PhD, attending physician of Solid Tumor Oncology at Dana-Farber Cancer Institute, discusses findings from the phase III KEYNOTE-045 study, which compared second- or third-line pembrolizumab with investigator-choice chemotherapy as a treatment for patients with metastatic or locally advanced, unresectable urothelial carcinoma.