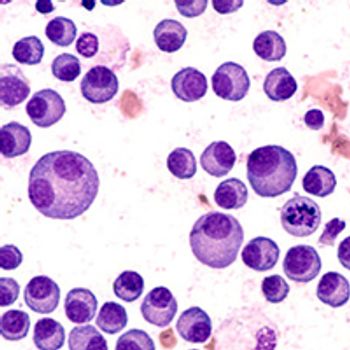
The novel SYK inhibitor cevidoplenib dosed at 400 mg twice per day led to robust platelet responses in patients with persistent or chronic primary immune thrombocytopenia who did not respond or relapsed after at least 1 prior therapy.

Your AI-Trained Oncology Knowledge Connection!

The novel SYK inhibitor cevidoplenib dosed at 400 mg twice per day led to robust platelet responses in patients with persistent or chronic primary immune thrombocytopenia who did not respond or relapsed after at least 1 prior therapy.
Ruxolitinib was found to improve spleen volume and tumor symptom score in patients with myelofibrosis, irrespective of their anemia and transfusion status, according to data from a post-hoc analysis of the phase 3 COMFORT-I and -II trials.

Although the event rate did reach the expected level and longer follow-up is needed to adequately assess long-term toxicities, data from the phase 3 IELSG37 trial support the omission of radiotherapy in patients with primary mediastinal large B-cell lymphoma who achieve a complete metabolic response following chemoimmunotherapy.

Patients with intermediate-2 or high-risk myelofibrosis who received the novel JAK/ACVR1 inhibitor jaktinib experienced a statistically significant improvement in the proportion of patients with a spleen-volume reduction of at least 35% from baseline at week 24 vs those who were treated with hydroxyurea.

Patients with primary or secondary TP53 wild-type myelofibrosis who experienced suboptimal response to ruxolitinib had clinically meaningful improvements in spleen volume reduction with the addition of navtemadlin to ruxolitinib,

The combination of the BCMA- and GPRC5D-targeted bispecific antibodies, teclistamab and talquetamab, respectively, demonstrated encouraging overall response rates and was well tolerated in patients with relapsed or refractory multiple myeloma.

The combination of daratumumab plus bortezomib, cyclophosphamide, and dexamethasone, elicited a complete response (CR) rate of 40% and a CR or better rate of 43% in patients with multiple myeloma presenting with extramedullary disease.

Daratumumab maintenance therapy with or without pomalidomide provided a tolerable and feasible treatment option after salvage hematopoietic stem cell transplantation in patients with relapsed multiple myeloma.
Teclistamab continued to elicit deep and durable responses in patients with relapsed/refractory multiple myeloma, irrespective of being triple-class refractory, daratumumab-refractory, or refractory to last line of therapy.
The addition of daratumumab to frontline induction therapy prior to peripheral blood stem cell collection reduced the number of patients with newly diagnosed multiple myeloma who were able to meet their stem cell collection goals on first attempt.

Treatment with ponatinib plus reduced-intensity chemotherapy led to an improvement in minimal residual disease-negative complete remission rate compared with imatinib plus reduced-intensity chemotherapy in newly diagnosed patients with Philadelphia chromosome-positive acute lymphoblastic leukemia.

Treatment with pelabresib monotherapy led to a 60% confirmed complete or partial hematologic response at any time without incurring grade 4 or 5 treatment-related adverse effects in patients with high-risk essential thrombocythemia refractory or intolerant to hydroxyurea.

The addition of acalabrutinib to bendamustine and rituximab demonstrated potent and durable responses despite a high incidence of grade 3/4 adverse effects in patients with previously untreated and relapsed/refractory mantle cell lymphoma.
The combination of daratumumab, ixazomib, and dexamethasone produced rapid and encouraging responses rates following lenalidomide–based therapy in patients with relapsed/refractory multiple myeloma, according to findings from the final analysis of the phase 2 DARIA trial.
Acalabrutinib is safe in patients with chronic lymphocytic leukemia who are at least 80 years of age and/or frail.

Patients with depression and/or anxiety prior to a diagnosis of diffuse large B-cell lymphoma had shorter survival times than patients without a mental health diagnosis.

Stephen V. Liu, MD, highlighted the importance of next-generation sequencing in lung cancer, key trials that have shifted the non–small cell lung cancer treatment landscape, and detailed ongoing research at Georgetown University Lombardi Comprehensive Cancer Center.

Although patients with metastatic nonseminomatous germ-cell tumors who had teratoma in the primary tumor were found to have a higher rate of teratoma in residual non-retroperitoneal disease following chemotherapy, those without teratoma in the primary tumor could have teratoma or active testicular germ-cell tumors in residual disease post-chemotherapy and should be considered for resection.
The FDA has removed a partial clinical hold that had been placed on a phase 1 trial investigating the safety and efficacy of MT-0169 as a potential therapeutic option in patients with relapsed or refractory multiple myeloma or non-Hodgkin lymphoma.

Looking to replicate the impressive findings with CAR T-cell therapies observed in patients with hematologic malignancies, investigators have initiated the BASECAMP-1 trial with the hope of identifying patients with advanced solid tumors who will be suitable candidates for treatment in the EVEREST trial.
Acalabrutinib and zanubrutinib demonstrated similar investigator-assessed progression-free survival in patients with relapsed/refractory chronic lymphocytic leukemia.

The FDA has accepted for review a supplemental biologics license application seeking the approval of pembrolizumab plus standard chemotherapy comprised of gemcitabine and cisplatin for use in patients with locally advanced unresectable or metastatic biliary tract cancer.

VCU Massey Cancer Center has been designated a Comprehensive Cancer Center by the National Cancer Institute, the nation’s principal authority on cancer research and training.

The addition of durvalumab to standard neoadjuvant chemotherapy significantly improved pathologic complete response over neoadjuvant chemotherapy alone in patients with resectable, early-stage and locally advanced gastric and gastroesophageal junction cancers.

The FDA has extended the Prescription Drug User Fee Act decision date by 3 months to allow more time to complete their review of the new drug application seeking the approval of nirogacestat in the treatment of adult patients with desmoid tumors.

A survey conducted by the National Comprehensive Cancer Network Best Practices Committee found that 93% of United States cancer centers polled in the report are experiencing a shortage of carboplatin, and 70% currently have a shortage of cisplatin.

Two-year follow-up data from the RELATIVITY-047 trial showed a continued benefit for patients with previously untreated, unresectable, or metastatic melanoma receiving nivolumab plus relatlimab vs nivolumab monotherapy supporting the use of the combination.

A supplemental biologics license application seeking the approval of ciltacabtagene autoleucel for use in adult patients with relapsed and lenalidomide-refractory multiple myeloma who have previously received at least 1 line of therapy, including a proteasome inhibitor and an immunomodulatory agent, has been submitted to the FDA.

Researchers at Fox Chase Cancer Center have developed a model that mimics patients’ tumor microenvironment that they believe has the potential to inform therapeutic decision making and presented a case study demonstrating the use of the model recently at the Atlantic Regional Hematopathology Meeting.
The first-in-class EGFR x HER3 bispecific antibody-drug conjugate BL-B01D1 generated antitumor activity and safety in patients with advanced solid tumors, particularly EGFR-mutated and wild-type non–small cell lung cancer and nasopharyngeal carcinoma.