Frontline treatment decisions for patients with follicular lymphoma can be guided by a general framework; the choice of therapy is often based on several factors such as indications of therapy, bulk of disease, comorbidities, and toxicity.

Your AI-Trained Oncology Knowledge Connection!

Frontline treatment decisions for patients with follicular lymphoma can be guided by a general framework; the choice of therapy is often based on several factors such as indications of therapy, bulk of disease, comorbidities, and toxicity.

The treatment landscape for multiple myeloma is poised to enter a new era of innovation with the development of therapies that target B-cell maturation antigen, which is highly expressed on plasma and MM cells.

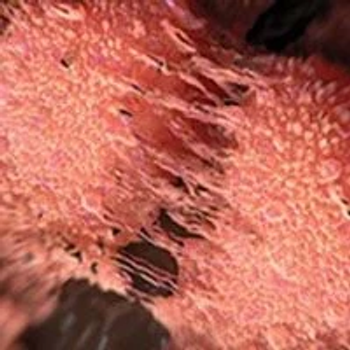
With an estimated 5-year survival rate of 50% and an ongoing issue of resistance, next steps with immunotherapy in melanoma will focus on stratifying patients, personalizing therapy, and refining localized regimens.

The addition of anti–PD-1/PD-L1 to combination BRAF and MEK inhibition has been shown to improve progression-free survival and duration of response in patients with BRAF-mutated melanoma, suggesting potential to overcome resistance to targeted approaches.

Jason J. Luke, MD, FACP, discusses the importance of BRAF in melanoma.

Jeffrey S. Weber, MD, PhD, discusses the results of the phase 3 COMBI-AD trial with dabrafenib plus trametinib in patients with resected, stage III BRAF V600E/K–mutant melanoma.

XmAb18087 demonstrated a disease control rate of 43% across dose levels in patients with neuroendocrine tumors and a favorable safety profile.

The novel somatostatin analog for the Targeted Alpha-emitter Therapy 212Pb-DOTAMTATE has demonstrated early efficacy and a tolerable safety profile in a small cohort of patients with metastatic somatostatin receptor–expressing neuroendocrine tumors irrespective of location of the primary tumor.

Aman Chauhan, MD, a medical oncologist at the University of Kentucky, discusses key recent advances in therapeutics for patients with neuroendocrine tumors, and points to the future with ongoing combination studies.

Increasing the dosage of lanreotide autogel from every 28 days to every 14 days led to encouraging progression-free survival outcomes in patients with progressive pancreatic and midgut neuroendocrine tumors.

Jonathan Strosberg, MD, discusses retreatment with Lutathera in advanced neuroendocrine tumors.

Aman Chauhan, MD, a medical oncologist at the University of Kentucky, discusses the role of Lutathera in neuroendocrine tumors.

Marianne Pavel, MD, discusses the progression-free survival of patients with pancreatic and midgut neuroendocrine tumors who are treated with lanreotide autogel in the phase 2 CLARINET FORTE trial.

Investigators are evaluating the combination of telotristat ethyl and Lutathera with a goal to improve progression-free survival in patients with well-differentiated neuroendocrine tumors in a randomized, phase 2 study that was highlighted during the 2020 NANETs Virtual Symposium.

Longer-term data demonstrated that treatment with the radiopharmaceutical Lutathera continued to show low rates of toxicity among patients with somatostatin receptor–positive neuroendocrine tumors.

Brigatinib demonstrated sustained improvements in overall and intracranial progression-free survival and health-related quality of life compared with crizotinib in patients with ALK-positive advanced non–small cell lung cancer.

Plinabulin was found to be a more favorable option for the prevention of chemotherapy-induced neutropenia compared with pegfilgrastim during the coronavirus disease 2019 pandemic.

Daniel P. Petrylak, MD, discusses the pivotal trials that have led to the regulatory approvals of the PARP inhibitors olaparib and rucaparib in patients with metastatic castration-resistant prostate cancer and DNA repair mutations.

Benjamin P. Levy, MD, discusses the role of the combination of dabrafenib and trametinib in BRAF V600E-mutant non–small cell lung cancer.

Andre Goy, MD, MS, discusses how matching the right treatment with the right patient resides at the heart of precision medicine, but with continued interest in pursuing the molecular milieu of cancers, precision medicine has the potential to better inform pre- and post-cancer interventions as well.

Despite efforts to advance the precision oncology portfolio for patients with diffuse large B-cell lymphoma by categorizing subtypes of the molecularly heterogenous disease, developing treatment routes for these alternate forms presents an uphill battle.

Although frontline chemoimmunotherapy regimens have been the gold standard for patients with chronic lymphocytic leukemia for many years, the advent of BTK inhibitors and other novel drugs has moved the field toward adopting chemotherapy-free options for patients in this setting.

Efforts to leverage targeted therapy and immunotherapy, which have been approved modalities in advanced non–small cell lung cancer, are leading to improved survival in patients with advanced and earlier-stage disease.

Andre Goy, MD, MS, discusses updates in precision medicine.
Natalie I. U. Vokes, MD, discusses the rise of predictive genomic biomarkers in oncology.

Over the past decade in gastrointestinal cancer treatment, the acknowledgement that cancer is heterogeneous and likely polyclonal has prompted a shift from gene testing for some patients, to many patients.

Natalie I. U. Vokes, MD, discusses investigative biomarkers of response to checkpoint inhibitors in the field of oncology.
With more than 4 years of follow-up, the health-related quality of life of men with nonmetastatic castration-resistant prostate cancer receiving androgen deprivation therapy was shown to be maintained with the addition of apalutamide.

Andrew B. Nixon, PhD, MBA, discusses the role of microsatellite instability in cancer.

Petros Grivas, MD, PhD, discusses findings from the subgroup analyses of JAVELIN Bladder 100 in advanced urothelial cancer.