
The combination of osimertinib and bevacizumab did not prolong progression-free survival in patients with advanced adenocarcinoma who had EGFR T790M mutations compared with osimertinib alone

Your AI-Trained Oncology Knowledge Connection!


The combination of osimertinib and bevacizumab did not prolong progression-free survival in patients with advanced adenocarcinoma who had EGFR T790M mutations compared with osimertinib alone

Overall survival benefits of frontline maintenance treatment with avelumab in patients with advanced urothelial cancer were found to be positively associated with biomarkers of immune activity and negativity linked with biomarkers of tumor homeostasis and chronic inflammation.

Quality of life according to patient-reported outcomes was not reduced despite treatment toxicities in those with ovarian, primary peritoneal, or fallopian tube cancer treated with niraparib versus placebo in the PRIMA/ENGOT-OV26/GOG-3012 trial.

The addition of abemaciclib to endocrine therapy led to a significant reduction in the risk of invasive disease versus endocrine therapy alone in patients with high-risk early hormone receptor–positive, HER2-negative breast cancer.

Post-operative radiotherapy was linked with a nonstatistically significant increase in disease-free survival in patients with completely resected stage IIIAN2 non–small cell lung cancer and thus cannot be recommended as a standard of care for this population.

Neoadjuvant chemotherapy with intense dose-dense epirubicin, paclitaxel, and cyclophosphamide demonstrated significant benefit in the treatment of patients with HR+/HER2- breast cancer.

The addition of neoadjuvant atezolizumab to nab-paclitaxel plus doxorubicin and cyclophosphamide significantly improved pathologic complete responses in patients with stage 2 or stage 3 triple-negative breast cancer, compared with placebo plus chemotherapy.

John Zalcberg, PhD, OAM, discusses updated results from the phase 3 INVICTUS trial in advanced gastrointestinal stromal tumor.

Benjamin Solomon, MBBS, PhD, FRACP, discusses interim findings from the phase 3 CROWN study in ALK-positive non–small cell lung cancer.

Dostarlimab showcased durable antitumor activity in patients with advanced or recurrent DNA mismatch repair deficient and proficient endometrial cancer, with a notable disease control rate and a promising safety profile.

Treatment with sacituzumab govitecan led to a 59% reduction in the risk of disease progression or death compared with physician’s choice of single-agent chemotherapy in patients with previously treated metastatic triple-negative breast cancer.
Sacituzumab govitecan-hziy continued to showcase significant activity with favorable tolerability in heavily pretreated patients with metastatic urothelial carcinoma who progressed on both platinum-based chemotherapy and checkpoint inhibition.
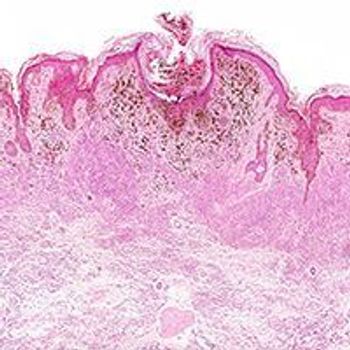
Spartalizumab plus dabrafenib did not significantly improve progression-free survival over dabrafenib/trametinib in patients with untreated BRAF V600-mutant unresectable or metastatic melanoma.

The novel broad-spectrum KIT and PDGFRα inhibitor ripretinib continued to demonstrate clinically meaningful benefit as a fourth- or later-line treatment for patients with advanced gastrointestinal stromal tumors.

Although the SOLAR-1 trial did not cross the prespecified O’Brien-Fleming efficacy boundary in postmenopausal patients with PIK3CA-mutant, hormone receptor–positive, HER2-negative advanced breast cancer, alpelisib and fulvestrant nevertheless prolonged the median OS.

Early findings from a phase II efficacy and safety study may be the first step in developing a definitive rationale for sequencing targeted therapies and immunotherapies in patients with metastatic melanoma.

Neither monotherapy with durvalumab or combination treatment with durvalumab plus tremelimumab met co-primary end points of overall survival vs chemotherapy for the treatment of metastatic urothelial cancer.

As first-line therapy for patients with microsatellite instability-high and/or mismatch-repair deficient metastatic colorectal cancer, pembrolizumab improves quality of life compared with standard chemotherapy.

The benefits conferred by the combination of nivolumab and ipilimumab for the first-line treatment of advanced renal cell carcinoma remained durable after 4-year follow-up compared with treatment with sunitinib.

Improvements in disease-free survival and progression-free survival were observed in patients with progressive pancreatic or midgut neuroendocrine tumors whose frequency of dosing for lanreotide Autogel was increased from 120 mg every 28 days to every 14 days.

Safety and preliminary antitumor activity with the bispecific antibody RO7122290 alone or in combination with atezolizumab demonstrated preliminary antitumor activity and was safe for the treatment of patients with advanced solid tumors.

The investigative PD-1 inhibitor balstilimab as a single agent and combined with the CTLA-4 inhibitor zalifrelimab showed promising objective response rates, regardless of PD-L1 expression, and a tolerable safety profile in patients with recurrent/metastatic cervical cancer.

Although atezolizumab did not improve pathological complete response when added to carboplatin and nab-paclitaxel, the immunotherapy increased the pCR by 10% or more in “immune-rich” groups with high-risk and locally advanced triple-negative breast cancer, and also turned PD-L1 negative tumors positive in most immunotherapy-treated patients.

The combination of nivolumab and cabozantinib led to a 49% reduction in the risk of disease progression or death, while also significantly improving overall survival and doubling objective response rate, compared with sunitinib in the first-line treatment of patients with advanced renal cell carcinoma.

Neoadjuvant durvalumab achieved a satisfactory complete surgical resection rate in patients with resectable non–small cell lung cancer, demonstrating preliminary promise for this treatment strategy.
One preoperative injection of atezolizumab was considered safe and induced major pathological responses in select patients with resectable non–small cell lung cancer.
Three-year follow-up data for the phase 2 study of the first-in-class inhibitor of apoptosis protein antagonist, xevinapant, in combination with standard cisplatin-based concomitant fractionation chemoradiation therapy reduced the risk of mortality by half compared with CRT alone in patients with locally advanced squamous cell carcinoma of the head and neck.

Frontline maintenance treatment with avelumab plus best supportive care improved both progression-free and overall survival compared with BSC alone across prespecified subgroups of patients with advanced or metastatic urothelial carcinoma that has not progressed on first-line platinum-based chemotherapy.

Despite observed responses, induction therapy with avelumab prior to standard of care gemcitabine/carboplatin fails to sustain clinically meaningful efficacy and is not an adequate strategy for the first-line treatment for patients with metastatic urothelial carcinoma.
The investigational PD-L1 inhibitor BGB-A333 in combination with the PD-1 inhibitor tislelizumab demonstrated marked antitumor activity, durable clinical responses, and a tolerable safety profile in patients with urothelial carcinoma.