Immunotherapy and You: Checkpoint Inhibitors in Gynecologic Cancers
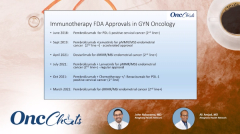
In this sixth episode of OncChats: Immunotherapy and You, John Nakayama, MD, and Ali Amjad, MD, highlight the success seen with checkpoint inhibitors in gynecologic cancers, biomarkers of interest, and recent approvals in the space.
Episodes in this series

In this sixth episode of OncChats: Immunotherapy and You, John Nakayama, MD, of the Division of Gynecologic Oncology, Allegheny Health Network, and assistant professor of OBGYN at Drexel University, and Ali Amjad, MD, medical hematologic oncologist, Allegheny Health Network, highlight the success seen with checkpoint inhibitors in gynecologic cancers, biomarkers of interest, and recent approvals in the space.
Nakayama: At this point, we've talked about mechanism action and a little bit about the history [of checkpoint inhibition], but I think [providing] an example might [make it] a little bit easier [to understand]. Since I'm a gynecologic oncologist, and I can't help myself, I think using [looking at this field] as an example would be good because we're very early in the process [of utilizing this approach], and we're trying to catch up to many of the medical oncologists [who are leveraging these agents].
In gynecologic oncology, [specifically] in ovarian cancer, it has been generally disappointing. We have had a lot of negative trials. There has been 1 trial that was sort-of positive but [data have not] been fully published yet. In cervical [cancer], we're really starting to see [the benefits of these agents]—especially [in those who have a] combined positive score of greater than 1%. When the trial that was looking at 4 different agents in cervical cancer [came out, I asked myself], is that the most you can get in any tumor? Is that a lot? How do these people tolerate this?
Amjad: That is certainly a lot. Certain [patients with this kind of] cancer are generally younger, so they have good organ function and they can tolerate all of it. However, since we have an effective combination, it's time to try to see whether we can do less and cut back to some degree [to achieve] a similar effect. [To that end,] there are clinical trials [that are] evaluating less cytotoxic chemotherapy and more immunotherapy and targeted treatments. Antibody-drug conjugates [are also] being evaluated in combination with immunotherapy.
Nakayama: Sure, and I think we will hit this with our next slide. Let's talk about endometrial cancer beyond [the] first-line [setting]. What is deficient mismatch repair? What is proficient mismatch repair?
Amjad: Mismatch repair deficiency by mismatch repair proteins are coded by genes called mismatch repair genes and these genes code for these DNA repair proteins, which are considered spell checks. As such, they would fix any errors in DNA replication. When a tumor is deficient in these proteins, DNA repair is not effective so new mutations develop. With those news mutations, there's neoantigens. Deficient mismatch repair seems to be a biomarker [that tells us that patient has] a better chance of responding to immunotherapy.
Nakayama: That has always made a lot of sense to me. I think a lot of this, if [a patient has] really poor DNA repair, [they are] spilling these antigens everywhere. As such, the antigen-presenting cells come along, and just have a lot more options to work with. That's the way it works. In my mind. Do you think [about this in a] similar [way]?
Amjad: Yeah, that's spot on.
Nakayama: Alright, and I see the percentages here. It looks like the majority of patients are mismatch repair proficient, which makes sense; everybody wants their DNA to work right.
The other really interesting thing that you brought up with this, is that we are looking at these 4 genes: MLH1, MSH2, MSH6, and PMS2. We actually screened every [patient with] endometrial cancer for that at the time of their surgery and their pathology to look for something like Lynch syndrome. Have you noticed that this changes your practice? Do you feel like everybody should be screened? Do you think we should be looking at tumor testing as opposed to looking at the mismatch repair genes?
Amjad: With this biomarker getting an FDA approval with tissue-agnostic treatments, every solid tumor should get tested for mismatch repair either [with immunohistochemistry] or next-generation sequencing. That is...what we do these days for almost all cancers.
Check back next Wednesday to view the next segment in this series.