Immunotherapy and You: Gynecologic Treatment Efficacy From a Patient’s Perspective
In this second episode of OncChats: Immunotherapy and You, John Nakayama, MD, and Ali Amjad, MD, discuss the safety and efficacy of immunotherapy vs standard chemotherapy in patients with gynecologic cancers.
Episodes in this series

In this second episode of OncChats: Immunotherapy and You, John Nakayama, MD, of the Division of Gynecologic Oncology, Allegheny Health Network, and assistant professor of OBGYN at Drexel University, and Ali Amjad, MD, medical hematologic oncologist, Allegheny Health Network, discuss the safety and efficacy of immunotherapy vs standard chemotherapy in patients with gynecologic cancers.
Nakayama: You mentioned checkpoint inhibition before. I think a confusion that a lot of people have is that there is more than one kind of immunotherapy, right?
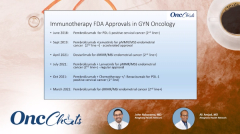
Amjad: That's correct. Immunotherapy is a general term. Checkpoint inhibition is just 1 subset of immunotherapy. People call vaccines immunotherapy, as well. Monoclonal antibodies can also be [referred to as] immunotherapy. However, we have seen a wave of checkpoint inhibitors being approved, [and these agents] improve the efficacy of the immune system. That is what immunotherapy refers to, for the most part.
Nakayama: So, at least from my standpoint, when I think about immunotherapy, I think about checkpoint inhibitors. [These agents] attack [the cancer] in a in a very different way, as opposed to cytotoxic chemotherapy. Could you talk a little bit about this, in terms of efficacy, from a patient's perspective?
Amjad: When we have a patient [with cancer who] comes to the office, the first question that they have for us—and the doctors think this way, as well—is [can their] cancer can be killed, and what will it take? Many times, when we talk about cancer treatments, [we think of] removing a cancer [and] addressing where it is right now. [We consider the] main treatment that can provide a cure for that cancer, and that would involve surgery or radiation treatments.
Then, there are adjuvant treatments, where you treat cancer after curative-intent surgery so that the risk of recurrence can be minimized. That's where, traditionally, we've used cytotoxic chemotherapy a lot. We still do, but recently, we've seen some studies that have shown immunotherapy as a very effective adjuvant treatment. In many cancers, [we have seen immunotherapy [perform] better than chemotherapy. To give you a few examples in lung cancer, in melanoma, in kidney cancer, and bladder cancer, we have immunotherapy approvals as adjuvant treatments.
Many times, these patients have cancers that are not curable; they are stage IV. The first thing that comes to mind from the patient's perspective, is that they want to start feeling better; they want to try to stay well and live longer. This is something that we [see] day in and day out. On clinical trials, when when we study these concepts, we capture a response rate. When tumors shrink, patients start feeling better. [With] immunotherapy, in many cases, if we have the right biomarker, [we] can [achieve] a very impressive response rate. In some cases, [the responses are] better than [what is seen with] chemotherapy. When these patients stay on therapy, and they have minimal adverse effects [AEs], they can be well for a long time and survive cancers for many years—even [those] with stage IV disease.
Nakayama: You mentioned something really interesting about toxicity. Have you found immunotherapy to be less toxic, the same, or more toxic, than standard cytotoxic chemotherapy?
Amjad: Certainly, [immunotherapy] is better tolerated. I tell my patients, 'When you're getting this cancer treatment, 8 or 10 times you will not notice that you are getting a medicine for cancer.' Patients certainly don't have the alopecia, nausea, and fatigue that comes with chemotherapy; [immunotherapy] does not affect the blood counts. However, there are going to be some patients who can have severe and unpredictable AEs from it; that can range from 2 to 3 out of 10 patients. Many of these AEs can be mild and manageable. As the saying goes, if anything ends with 'itis,' it can happen with immunotherapy. [Effects] like colitis, thyroiditis, endocrinopathies, pneumonitis [are being watched for] really, really closely. However, for the most part, patients do really well on this treatment.
Nakayama: Yeah, that has been my experience. I'm a kind of a simple guy, and way that I think about it, [is] like you said, [in terms of] the -itises, inflammation or whatnot. My wife has has autoimmune disease, and in my mind, somehow it's like you're turning up that immune system a little more and it's almost like an autoimmune kind of thing. I recognize it's not the same, but you're turning it up, and you can have that -itis, that inflammation, anywhere; it can be any organ system. Maybe that's too simplistic, but that's the way that I think about it.
Amjad: No, I think you're right. The immune system has checks and balances. There are stop signals everywhere, and that's how the immune system is designed. If you have an infection, once the infection is eradicated, the immune system is supposed to calm down. As such, what we try to do here, is activate the immune system against the cancer, which can go the wrong direction, as well. The T cells can activate against the normal antigens, too; that is a real risk.
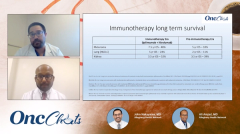
Nakayama: [Earlier, you were] talking about duration of response [with immunotherapy]; that caught my attention. I feel like, at least in gynecologic oncology, we have seen relatively low response rates. However, what has kept everyone super interested is the people who respond seem to have really long durations [of response]. Is that in other cancers as well, or is this a gynecologic phenomenon?
Amjad: No, that is true. You know, when you [use] immunotherapy, many times you create this equilibrium between the cancer and the tumor cells, to the degree that we sometimes see disease on a scan that seems to be dormant and doesn't seem to activate or progress as if a cancer would progress. So somehow, we change the behavior of a cancer and the cancer can live with the the body without having any major AEs.
Nakayama: I think it makes sense, those checks and balances, because tumors create an immunosuppressive environment. If you can alter [those] checks and balances, maybe you can keep it in check, like you are saying.
Amjad: That is correct. We'll talk more about PD-L1 and PD-1 blockers, but what happens is, cancer cells know how to hide from the immune system, and all we have to do is to try to expose them to the T cells, and that does the job.
Check back next Wednesday to view the next segment in this series.