Articles by Gina Columbus
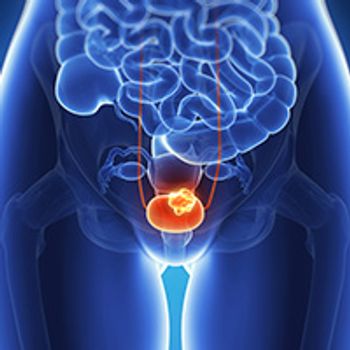
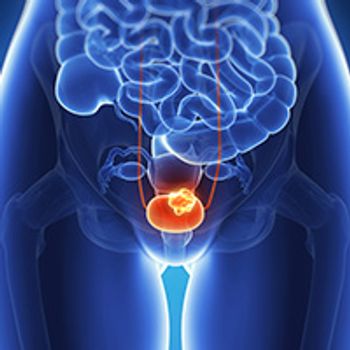
The United Kingdom’s National Institute for Health and Care Excellence has chosen not to recommend pembrolizumab as a treatment for patients with locally advanced or metastatic urothelial carcinoma who have previously received platinum-containing chemotherapy.

The FDA has placed a partial clinical hold on a phase I trial assessing the autologous T-cell therapy ACTR707 in combination with rituximab for patients with CD20-positive, B-cell non-Hodgkin lymphoma due to a safety concern.

The FDA has granted an accelerated approval to the combination of nivolumab and ipilimumab for the treatment of patients with hepatocellular carcinoma who have received prior therapy with sorafenib.

The FDA has granted a breakthrough therapy designation to JNJ-61186372 for the treatment of patients with EGFR-positive metastatic non–small cell lung cancer who harbor exon 20 insertion mutations, and whose disease has progressed on or after platinum-based chemotherapy.

The triplet therapy of ixazomib, lenalidomide, and dexamethasone showed an improvement in progression-free survival, but it was not statistically significant, compared with lenalidomide/dexamethasone alone for patients with newly diagnosed multiple myeloma who were ineligible for stem cell transplant.

The addition of elotuzumab to lenalidomide and dexamethasone did not show a statistically significant improvement in progression-free survival compared with lenalidomide/dexamethasone alone in patients with newly diagnosed, previously untreated, transplant-ineligible multiple myeloma.

Durvalumab alone did not improve overall survival compared with standard-of-care chemotherapy in patients with unresectable urothelial cancer whose tumors had high levels (≥25%) of PD-L1 expression, missing both primary endpoints of the phase III DANUBE trial.

The FDA has accepted a biologics license application for a proposed biosimilar for bevacizumab.

The FDA has granted a breakthrough device designation to the Elecsys GALAD score, an algorithmic score designed to aid in the diagnosis of early-stage hepatocellular carcinoma.

The FDA has granted a Fast Track Designation to tipifarnib for the treatment of adult patients with relapsed/refractory angioimmunoblastic T-cell lymphoma, follicular T-cell lymphoma, and nodal peripheral T-cell lymphoma with T follicular help phenotype.

The FDA has approved isatuximab-irfc (Sarclisa) for use in combination with pomalidomide (Pomalyst) and dexamethasone for the treatment of adult patients with multiple myeloma who have received ≥2 prior therapies, including lenalidomide and a proteasome inhibitor.

Selinexor in combination with bortezomib and low-dose dexamethasone led to a statistically significant increase in progression-free survival compared with bortezomib/dexamethasone alone in patients with multiple myeloma who have received 1 to 3 prior lines of therapy.

The FDA has granted a priority review designation to a biologics license application for the combination of tafasitamab and lenalidomide for the treatment of patients with relapsed/refractory diffuse large B-cell lymphoma.

Pembrolizumab demonstrated a statistically significant and clinically meaningful improvement in progression-free survival compared with brentuximab vedotin in adult patients with relapsed/refractory classic Hodgkin lymphoma, meeting one of the dual primary endpoints of the phase III KEYNOTE-204 trial.

With the main toxicities associated with CAR T-cell therapy being cytokine release syndrome and neurotoxicity, a multidisciplinary approach is vital to providing inclusive care to patients receiving this type of treatment.

The United Kingdom’s National Institute for Health and Care Excellence has recommended the combination of lenalidomide and rituximab as a treatment option for adult patients with grade 1 to 3A previously treated follicular lymphoma.

The FDA has granted a breakthrough therapy designation to Debio 1143, an inhibitor of apoptosis protein antagonist, for the treatment of patients with previously untreated, unresectable, locally advanced squamous cell carcinoma of the head and neck in combination with standard cisplatin-based concomitant fractionation chemoradiation therapy

The European Medicines Agency has validated a Type II Variation for niraparib as a first-line maintenance treatment for patients with advanced ovarian cancer who have responded to platinum-based chemotherapy, regardless of biomarker status.

The FDA's Oncologic Drugs Advisory Committee voted 6 to 5 in favor of intravenous ramucirumab injection for use in combination with erlotinib as a frontline treatment for patients with metastatic non–small cell lung cancer whose tumors harbor EGFR exon 19 deletions (Ex19del) or exon 21 (L858R) substitution mutations.

The FDA has approved a supplemental new drug application for neratinib in combination with capecitabine for the treatment of adult patients with advanced or metastatic HER2-positive breast cancer who have received ≥2 prior anti–HER2-based regimens in the metastatic setting.

The FDA has granted a priority review designation to a supplemental new drug application for selinexor as a treatment for adult patients with relapsed/refractory diffuse large B-cell lymphoma, not otherwise specified, who have received ≥2 prior therapies.

The FDA has issued a complete response letter to 6 supplemental biologics license applications that would have updated the dosing schedule for pembrolizumab to include an every-6-weeks option at 400 mg over 30-minute infusions across multiple indications.

The FDA has granted a breakthrough therapy designation to the combination of enfortumab vedotin-ejfv and pembrolizumab as a first-line treatment of patients with unresectable locally advanced or metastatic urothelial cancer who are unable to receive cisplatin-based chemotherapy.

The FDA has granted a priority review designation to a supplemental biologics license application for single-agent atezolizumab as a frontline treatment for patients with advanced nonsquamous or squamous non–small cell lung cancer without EGFR or ALK mutations who have high PD-L1 expression on tumor cells or tumor-infiltrating immune cells, defined as TC3/IC3 wild-type.

The combination of cabozantinib and atezolizumab demonstrated clinically meaningful activity in patients with metastatic castration-resistant prostate cancer, including those with high-risk clinical features.

The combination of nivolumab and the investigational CSF-1R inhibitor cabiralizumab with and without chemotherapy did not improve progression-free survival compared with chemotherapy alone in patients with advanced pancreatic cancer, missing the primary endpoint of a phase II trial (NCT03336216).

The FDA has granted a priority review designation to a new drug application for lurbinectedin as a treatment for patients with small cell lung cancer who have progressed following platinum-containing therapy.

The addition of the off-the-shelf cancer immune primer ilixadencel to sunitinib trended toward a benefit in overall survival compared with sunitinib alone as a first-line treatment for patients with newly diagnosed metastatic renal cell carcinoma.

The frontline combination of pembrolizumab and chemotherapy significantly improved progression-free survival compared with chemotherapy alone in patients with metastatic triple-negative breast cancer whose tumors expressed PD-L1.
Enzalutamide plus androgen deprivation therapy demonstrated a statistically significant improvement in overall survival compared with placebo/ADT in patients with nonmetastatic castration-resistant prostate cancer.