
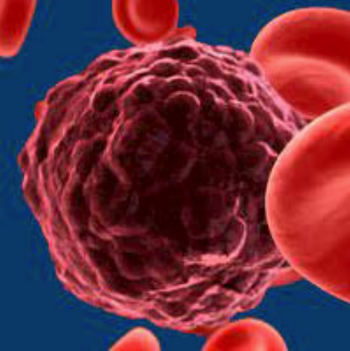
Single-agent ibrutinib given in the first-line setting sustained a progression-free survival and overall survival benefit compared with chlorambucil as therapy for patients with chronic lymphocytic leukemia at 7-year follow-up.

Your AI-Trained Oncology Knowledge Connection!


Single-agent ibrutinib given in the first-line setting sustained a progression-free survival and overall survival benefit compared with chlorambucil as therapy for patients with chronic lymphocytic leukemia at 7-year follow-up.

Zenocutuzumab represents a promising novel targeted therapeutic option for patients with NRG1 fusion–positive cancers.

Treatment with aumolertinib was associated with prolonged survival and duration of response in patients with non–small cell lung cancer.

Patients with relapsed/refractory diffuse large B-cell lymphoma treated with a novel combination of polatuzumab vetodin, rituximab and lenalidomide contributed to an improved overall response and complete response, with 82% remaining in remission at the study’s cutoff date.

Sylvie Bonvalot, MD, PhD, HDR, discusses the long-term safety of NBTXR3 plus radiotherapy in patients with locally advanced soft tissue sarcoma who were treated in the phase 2/3 Act.In.Sarc trial.
Allogeneic hematopoietic cell transplantation was safe when used with a reduced-intensity conditioning regimen of bortezomib, fludarabine, and melphalan in patients with high-risk multiple myeloma.

Sotorasib provided continued durable clinical benefit in patients with pretreated KRAS p.G12C–mutated non–small cell lung cancer.

A single infusion of brexucabtagene autoleucel, a CAR T-cell therapy, demonstrated robust and durable responses in heavily pretreated patients with relapsed/refractory B-cell acute lymphoblastic leukemia.

Amivantamab in combination with lazertinib elicited responses in more than one-third of chemotherapy-naïve patients with EGFR-mutant non–small cell lung cancer who had progressed on osimertinib.

The addition of lifileucel to pembrolizumab resulted in an overall response rate of 85.7% compared with pembrolizumab alone in patients with immune checkpoint inhibitor–naïve advanced melanoma.

Encouraging initial durability has been observed with afamitresgene autoleucel in patients with advanced synovial sarcoma or myxoid/round cell liposarcoma, according to data from the phase 2 SPEARHEAD-1 trial.

Patritumab deruxtecan was found to induce clinically meaningful, durable efficacy in heavily pretreated patients with EGFR-mutated non–small cell lung cancer who were resistant to EGFR TKIs.

Catequentinib improved disease control and progression-free survival in patients with advanced synovial sarcoma compared with dacarbazine.

Ferdinandos Skoulidis, MD, PhD, MRCP, discusses the results of subgroup analysis from the phase 2 CodeBreaK 100 trial in patients with KRAS G12C-mutant non–small cell lung cancer.

The efficacy demonstrated with combination of ponatinib and blinatumomab represent a potentially promising chemotherapy-free, hematopoietic stem cell transplant–sparing treatment for patients with Philadelphia chromosome–positive acute lymphocytic leukemia.

Martin Reck, MD, PhD, discusses updated results of the phase 3 CheckMate 9LA study in advanced non–small cell lung cancer.

The investigational SHP2 inhibitor TNO155 demonstrated encouraging safety and tolerability, and consistent evidence of SHP2 inhibition in patients with advanced solid tumors.
Evidence of tucatinib and its predominant metabolite, ONT-993, were detectable in the cerebrospinal fluid of patients with leptomeningeal metastasis HER2+ positive breast cancer marking a first for tucatinib distribution into the CSF seen in this patient population.

Toni K. Choueiri, MD, discusses the efficacy of pembrolizumab as a post-nephrectomy adjuvant therapy for patients with renal cell carcinoma from the phase 3 KEYNOTE-564 trial.

Nivolumab and ipilimumab plus 2 cycles of platinum-based chemotherapy demonstrated durable survival benefit vs chemotherapy alone in patients with advanced non–small cell lung cancer.

CLN-081 demonstrated promising preliminary antitumor activity and an acceptable safety profile across all doses tested in patients with previously treated non–small cell lung cancer (NSCLC) harboring EGFR exon 20 insertion mutations.

Tivozanib led to a more than doubled median duration of response compared with sorafenib in patients with metastatic renal cell carcinoma.

Avelumab as frontline maintenance plus best supportive care demonstrated a survival benefit compared with BSC alone across several previously unreported subgroups of patients with advanced urothelial cancer who have progressed on first-line platinum-containing chemotherapy.

Data from an updated analysis of the phase 3 PACIFIC trial indicate that treatment with durvalumab after chemoradiotherapy is associated with long-term survival improvements in patients with unresectable stage III non-small cell lung cancer.

The combination of nivolumab and ipilimumab continued to provide a durable, long-term overall survival benefit compared with chemotherapy after 4 years for patients with advanced non‒small cell lung cancer regardless of PD-L1 expression or histology.

Cirmtuzumab and ibrutinib led to reported high overall response rates in patients with mantle cell lymphoma or chronic lymphocytic leukemia.

The tri-specific half-life extended prostate-specific membrane antigen-targeting T cell engager HPN424 demonstrated antitumor activity and was well tolerated in patients with metastatic castration-resistant prostate cancer.

Mobocertinib, a first-in-class, oral, EGFR TKI, induced rapid, deep, and durable responses and a manageable safety profile in patients with platinum-pretreated EGFR exon 20 insertion–positive metastatic non–small cell lung cancer.

Deep and early responses were yielded with a single infusion of ciltacabtagene autoleucel in patients with previously treated, relapsed/refractory multiple myeloma.

Pembrolizumab plus concurrent chemoradiation therapy induced antitumor effects in patients with unresectable, locally advanced, stage III non–small cell lung cancer irrespective of PD-L1 expression or tumor histology.