Natalie Callander, MD, discusses the role of ALC monitoring in the management of relapsed/refractory multiple myeloma following CAR T-cell therapy.

Your AI-Trained Oncology Knowledge Connection!


Natalie Callander, MD, is a professor in the Division of Hematology, Medical Oncology, and Palliative Care in the Department of Medicine at the University of Wisconsin (UW) School of Medicine and Public Health; as well as the director of the Myeloma Clinical Program at the UW Carbone Cancer Center.
Natalie Callander, MD, discusses the role of ALC monitoring in the management of relapsed/refractory multiple myeloma following CAR T-cell therapy.

Panelists discuss how community providers can implement strategies and utilize resources to effectively connect patients to referral centers for chimeric antigen receptor T-cell therapy, while addressing how to initiate conversations about the therapy and counsel patients regarding potential adverse events.

Panelists discuss how early referral for chimeric antigen receptor T-cell therapy is crucial for patients, as it helps to overcome potential barriers and ensures timely access to this transformative treatment option.

Panelists discuss how patient and disease factors influence the choice between ide-cel and cilta-cel for chimeric antigen receptor (CAR) T-cell therapy, the significance of adverse event profiles in clinical decision-making, the use of bridging therapy prior to infusion, and the experiences of progression rates and potential mechanisms post treatment, as well as future directions for CAR T-cell therapy in relapsed/refractory multiple myeloma.

Panelists discuss how the KARMMA-3 study’s design, patient population, and efficacy outcomes—including overall survival data—inform the approval of ide-cel, as well as the implications of CARTITUDE-4’s recent findings on treatment selection and approaches for cilta-cel in chimeric antigen receptor T-cell therapy.

Panelists discuss the currently available chimeric antigen receptor T-cell therapies for early relapse multiple myeloma, examining their place within the treatment paradigm and how factors such as product type (cilta-cel vs ide-cel) and high-risk features (such as minimal residual disease positivity post induction and extramedullary disease) influence clinical decision-making.

Panelists discuss the key disease and patient factors considered when choosing between triplet and quadruplet induction regimens for patients with transplant-ineligible multiple myeloma, as well as the unmet needs that persist in the treatment landscape for both transplant-eligible and ineligible populations.

Panelists discuss the CEPHEUS trial results for newly diagnosed patients who are not transplant eligible, highlighting key takeaways. They also compare the CEPHEUS data with other quadruplet regimens in the non–transplant-eligible space, such as Isa-VRd.

Panelists discuss the importance of minimal residual disease negativity as a primary outcome measure and the treatment strategies for patients who are eligible for transplantation but choose to decline it, including preferred induction regimens for this population.

Panelists discuss whether daratumumab quadruplet induction regimens should be considered the new standard of care for newly diagnosed transplant-eligible patients and explore scenarios in which a triplet induction regimen might still be appropriate. They also review the findings from the ISKIA and GMMG-CONCEPT trials, including considerations for using isatuximab-carfilzomib (IsaKRd) over D-VRd.

Panelists discuss the findings of the PERSEUS trial and the recent cytogenetic risk analysis for patients with newly diagnosed transplant-eligible multiple myeloma. They then explore the CASSIOPEIA trial and its implications regarding daratumumab quadruplet induction regimens.
Considerations for optimizing treatment with BCMA-targeting agents for patients with relapsed/refractory multiple myeloma moving forward.
Current combination approaches, including BCMA-targeting agents like belantamab mafodotin, being explored to address treatment gaps in relapsed/refractory multiple myeloma.
An overview of novel bispecific therapies under development in relapsed/refractory multiple myeloma.
Implications for treating patients with relapsed/refractory multiple myeloma with CAR T cells vs antibody-drug conjugates.
Recommendations for managing ocular toxicities associated with belantamab mafodotin when used as treatment for relapsed/refractory multiple myeloma.
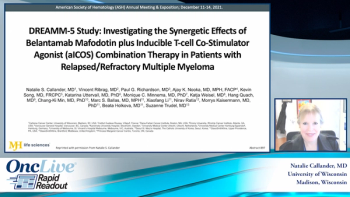
Dr. Natalie Callander reviews data from the DREAMM-5 study presented at ASH 2021, which assessed the safety and efficacy of belantamab mafodotin plus feladilimab in patients with relapsed/refractory multiple myeloma with disease resistance to at least 3 prior lines of therapy.
What to know in terms of dosing belantamab mafodotin treatment in patients with relapsed/refractory multiple myeloma.
Variables that impact treatment decisions for relapsed/refractory multiple myeloma.
Natalie Callander, MD, presents the profile of a female patient with relapsed/refractory multiple myeloma who receives belantamab mafodotin and develops keratopathy.
Karen L. Klugo, MD, describes what’s unique in terms of patient response to belantamab mafodotin as treatment for relapsed/refractory multiple myeloma and risk of ocular disease.
The rationale for treating relapsed/refractory multiple myeloma with belantamab mafodotin, and studies investigating the drug’s potential in earlier treatment settings.
Sagar Lonial, MD, FACP, highlights a novel treatment option available for a 57-year-old man whose disease progresses after 3 prior lines of therapy, including an immunomodulatory drug, a proteasome inhibitor, and an anti-CD38 antibody.
Published: February 28th 2022 | Updated:
Published: February 28th 2022 | Updated: