
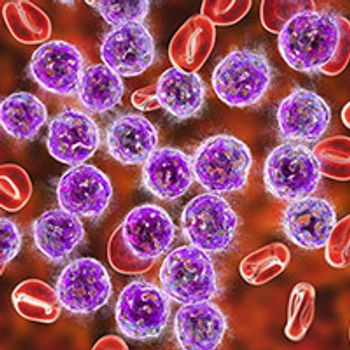
Mortality rates in patients with acute myeloid leukemia, acute lymphoblastic leukemia, and myelodysplastic syndrome who were diagnosed with COVID-19 were higher compared with non-cancer populations who were infected with the virus.

Your AI-Trained Oncology Knowledge Connection!


Mortality rates in patients with acute myeloid leukemia, acute lymphoblastic leukemia, and myelodysplastic syndrome who were diagnosed with COVID-19 were higher compared with non-cancer populations who were infected with the virus.

Maurie Markman, MD, discusses how agency leaders should be encouraged to improve regulatory science, include a patient’s perspective in approval decisions, reduce unnecessary bureaucracy and costs associated with the conduct of trials, and accelerate the overall review process for drug approval.
Telemedicine solidified its role as a new standard in patient care during the COVID-19 pandemic.
Three doses of the SARS-CoV2 vaccine were shown to be safe and effective in patients with lung cancer, particularly in those with minimal serologic response after receiving only 2 doses.

Patients with lymphoid malignancies, especially those who have received recent anti-CD20 antibody therapy, have reduced humoral responses to the mRNA COVID-19 vaccines, and as such, should continue to take precautionary measures against COVID-19 infection irrespective of vaccination status.

Although mortality rates in patients with hematologic cancers who develop breakthrough COVID-19 cases after vaccination are high, there has been a significant decrease in incidence since vaccines have become available.

Although community oncologists and hematologists were concerned about loss of income during the COVID-19 pandemic, the loss of in-person patient interaction was cited as the key factor impacting their professional satisfaction.

The COVID-19 vaccine was safe and well tolerated in patients who received immune checkpoint inhibitors for renal cell carcinoma or melanoma.

As the COVID-19 pandemic persists, patients with cancer should receive the full vaccination with 1 of the 3 approved COVID-19 vaccines as soon as they are able, according to Steven Ludlow, PharmD, BCOP, BCPS.

Routine computed tomography-based imaging scans identified abnormal ground-glass opacities and infiltrates indicative of COVID-19 in patients with lung cancer undergoing radiation therapy, enabling earlier diagnosis, treatment, and risk reducing measures.
Although CAR T-cell therapies have demonstrated unprecedented activity in patients with heavily pretreated relapsed/refractory hematologic malignancies, they are marked by a significant risk of infections and may limit the efficacy of COVID-19 vaccines.

A proportion of patients with multiple myeloma receiving CD38-directed and BCMA-directed therapies had a lack of T-cell responses and an absence of anti–SARS-CoV-2 Spike antibodies following SARS-CoV-2 vaccination, underscoring the need for serological testing after vaccination to identify these patients.

Maurie Markman, MD, highlights the ongoing regulatory concerns that demand attention of the FDA in the cancer arena amidst evolving issues regarding COVID-19.

Approximately 20% of pediatric patients with cancer infected with COVID-19 experienced severe illness and deaths due to the infection were proportionally higher in this patient population compared with the general pediatric population, providing evidence that children with cancer are at higher risk of developing severe illness from COVID-19.

Dr. Abid discusses immune-compromising factors that are indigenous to CAR T-cell therapy recipients, the immunogenic potential of different COVID-19 vaccines, determinants of vaccine responses, and the potential need for booster vaccine dosing in this population.

Muhammad Bilal Abid, MD, MRCP, discusses the potential impact of CAR T-cell therapy on the efficacy of COVID-19 vaccinations.
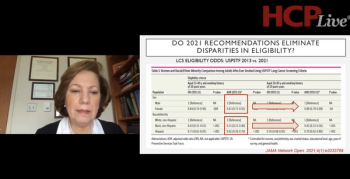
M. Patricia Rivera, MD, a professor of medicine at The University of North Carolina at Chapel Hill, reviews the United States Preventive Services Task Force's lung cancer screening recommendations as of 2021, including the impacted patient populations and effect the recommendations have on direct physician care.

Andrea Borondy Kitts, a lung cancer and patient advocate at Rescue Lung Society, educates physicians on adequate physician-to-patient education and resources that improve their opportunity for success in lung cancer care.
Jacob Sands, MD, a physician at Dana-Farber Cancer Institute, as well as an instructor of medicine at Harvard Medical School, describes the last decade in lung cancer diagnostics and significant therapeutic advances. He also navigates the emerging classes of drugs that are beginning to make headway in the lung cancer pipeline.
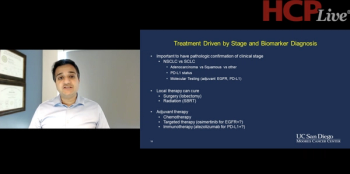
Sandip Patel, MD, an associate professor of medical oncology at University of California San Diego, explains the optimal diagnostic strategies that can be utilized to better inform biomarker-based therapies in lung cancer.
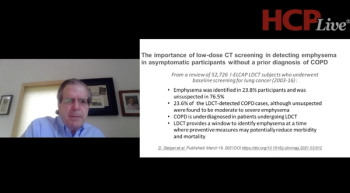
James L. Mulshine, MD, professor of internal medicine, and associate director of Institute of Translation Medicine at Rush University, discusses the benefits of establishing a timely and investigation-informed screening and referral practice for patients who are at risk for developing lung cancer.

The continued uncertainties of the current and future status of the COVID-19 pandemic have resulted in a lack of trust in the authority of the scientific establishment in the United States, and elsewhere, as it operates during these difficult times.

Six months after receiving a second dose of the Pfizer-BioNTech COVID-19 vaccine, patients with solid tumors retained similar levels of COVID-19 antibodies in their blood as individuals without cancer.

Clinical trial enrollments underwent a substantial decrease during the first year of the COVID-19 pandemic only to rebound during the winter 2020 to 2021 wave, and primarily affected enrollment to cancer control and prevention trials vs treatment trials.

Zev A. Wainberg, MD, discusses the importance of enrolling patients with colorectal cancer to clinical trials, despite the difficulties caused by COVID-19.
COVID-19 continued to result in high admission and fatality rates among patients with chronic lymphocytic leukemia during the first 13 months of the pandemic, and although risk of severe infection was determined to be independent of age, CLL status, and treatment, being age 75 years or older was revealed to be a significant risk factor for death.

A survey of more than 6,800 cancer patients conducted this month by Florida Cancer Specialists & Research Institute found that patients overwhelmingly prefer that the FCS physicians, nurses and staff members who provide their care are vaccinated and wear masks to reduce the spread of COVID-19 and provide a safe environment within clinics.

The National Comprehensive Cancer Center Network has issued an official statement calling on all healthcare systems to ensure that their workforces are immunized with one of the authorized COVID-19 vaccines.

The FDA has approved the Pfizer-BioNTech COVID-19 vaccine for use in the prevention of COVID-19 disease in individuals aged 16 years or older.

Chris Labaki, MD, and Quoc-Dien Trinh, MD, discuss their research on the decline in cancer screenings during the height of the COVID-19 pandemic, the recovery of these tests, and potential existing disparities to be addressed.