MRD as detected by a novel tumor-informed ctDNA assay helped identify patients with TNBC who were at higher risk for distant recurrence after surgery.

Your AI-Trained Oncology Knowledge Connection!

MRD as detected by a novel tumor-informed ctDNA assay helped identify patients with TNBC who were at higher risk for distant recurrence after surgery.

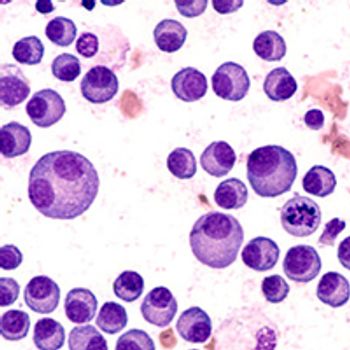
Zanubrutinib plus venetoclax maintained a 36-month PFS rate of 87% (95% CI, 78.6%–92.4%) in treatment-naive CLL/SLL.

Lisaftoclax demonstrated efficacy and safety for the treatment of patients with relapsed/refractory CLL/SLL.

Sirexatamab plus bevacizumab shows promise in improving survival for patients with DKK1-high metastatic colorectal cancer.
Enzalutamide plus leuprolide acetate led to a 40.3% lower risk of death vs leuprolide acetate alone in high-risk, biochemically recurrent prostate cancer.
The addition of disitamab vedotin to toripalimab and trastuzumab and/or CAPOX led to favorable response rates in HER2-expressing gastric/GEJ cancer.
Runimotamab in combination with trastuzumab led to clinical activity and tolerability vs runimotamab alone in HER2-positive breast cancer.
Nogapendekin alfa inbakicept demonstrated sustained CR rates in patients with high-risk BCG-unresponsive NMIBC.

SHR-A1811 monotherapy demonstrated high clinical activity and was well tolerated in patients with HER2-positive breast cancer.
Pirtobrutinib improved progression-free survival in previously treated chronic lymphocytic leukemia and small lymphocytic lymphoma.

Radium-223 prior to docetaxel improved quality of life and tolerability in patients with metastatic castration-resistant prostate cancer according to data from the RAPSON trial.

Neha Mehta-Shah, MD, MSCI, discusses unmet needs and future developments in the treatment of patients with peripheral T-cell lymphoma.

Elias Jabbour, MD, discusses the potential activity and financial benefit of novel and emerging TKIs for first-line management of chronic phase CML.

The investigation of treatments harnessing the immune system in patients with T-cell lymphoma could lead to "a new era" of therapy for this patient population.

The administration of CAR T-cell therapy in the outpatient setting was deemed feasible and safe in patients with relapsed/refractory NHL.

In patients with NSCLC refractory to anti-PD(L)1 therapy, CAN-2409 (adenovirus) plus valacyclovir co-administered with ICI therapy showed acceptable tolerability and potential for immune modulation

Concurrent radical cystectomy and extended lymph node dissection did not show benefit vs standard lymph node dissection in muscle invasive urothelial cancer.

Neoadjuvant tislelizumab in combination with chemotherapy was safe and produced responses in patients with locally advanced cervical cancer.

Adjuvant chemotherapy did not improve circulating tumor DNA clearance in patients with stage II colon cancer with baseline circulating tumor DNA.
The presence of molecular minimal residual disease following induction chemotherapy can be used to determine patients with NPM1-mutated acute myeloid leukemia who may benefit from allogeneic transplant in first remission, including those with FLT3 ITD–mutated disease.

Treatment with subcutaneous epcoritamab-bysp elicited rapid and durable responses, including an encouraging complete response rate, and manageable safety in high-risk patients with relapsed/refractory chronic lymphocytic leukemia.

Forimtamig monotherapy generated high overall response rates and durable responses in all subgroups of patients with relapsed/refractory multiple myeloma enrolled in a phase 1a dose-escalation trial.

Developing an optimal treatment strategy for patients with accelerated- or blast-phase myeloproliferative neoplasms requires consideration of a patient's ability to tolerate intensive induction therapy, their eligibility for allogeneic stem cell transplant.

Investigating the addition of novel agents to cytotoxic chemotherapy may help prevent relapse in patients with T-cell acute lymphoblastic leukemia by bolstering the efficacy of these standard frontline therapies.

Ibrutinib did not prolong survival vs placebo and is linked with increased susceptibility to bleeding in patients with asymptomatic early-stage chronic lymphocytic leukemia, suggesting that a watch-and-wait approach should continue as the standard for this population.
The addition of daratumumab to frontline induction therapy prior to peripheral blood stem cell collection reduced the number of patients with newly diagnosed multiple myeloma who were able to meet their stem cell collection goals on first attempt.

Treatment with doxorubicin plus zalifrelimab and balstilimab produced a favorable 6-month progression-free survival rate in patients with difficult-to-treat soft tissue sarcoma subtypes unlikely to respond to doxorubicin or immune checkpoint inhibitor monotherapy.

The CAR T-cell therapy PHE885 produced responses and high minimal residual disease negativity rates with no new safety signals in patients with relapsed/refractory multiple myeloma.

Second-line atezolizumab plus cabozantinib did not generate a clinical benefit over standard-of-care docetaxel in patients with metastatic non–small cell lung cancer previously treated with immune checkpoint inhibitors and chemotherapy.

Pembrolizumab plus standard-of-care chemotherapy, followed by maintenance pembrolizumab, reduced the risk of disease progression or death vs chemotherapy alone in patients with mismatch repair–deficient and mismatch repair–proficient advanced or recurrent endometrial cancer.

Published: December 8th 2022 | Updated:

Published: December 9th 2021 | Updated:

Published: June 5th 2022 | Updated:

Published: September 20th 2020 | Updated:
Published: March 20th 2021 | Updated:

Published: December 6th 2020 | Updated: