
The combination of bevacizumab (Avastin) and erlotinib (Tarceva) is superior to erlotinib alone as upfront treatment for non–small cell lung cancer harboring EGFR mutations.

Your AI-Trained Oncology Knowledge Connection!


The combination of bevacizumab (Avastin) and erlotinib (Tarceva) is superior to erlotinib alone as upfront treatment for non–small cell lung cancer harboring EGFR mutations.

The investigational second-generation tyrosine kinase inhibitor dacomitinib improved overall survival compared with gefitinib as first-line treatment in patients with advanced non-small cell lung cancer harboring activating EGFR mutations.

The pathologic complete response rate associated with the trastuzumab biosimilar ABP 980 was equivalent to that of reference trastuzumab based on central laboratory evaluation in patients with HER2-positive early breast cancer enrolled in the phase III LILAC study.

MYL-1401O (Ogivri; trastuzumab-dkst) added to a taxane as initial therapy followed by MYL-1401O monotherapy as maintenance resulted in a nearly identical rate of progression-free survival compared with trastuzumab (Herceptin) in patients with HER2-positive metastatic breast cancer.

The bevacizumab biosimilar PF-06439535 demonstrated similarity to the European Union bevacizumab reference product for overall response rate, with similar pharmacokinetic and immunogenicity profiles for patients with advanced non-squamous non-small cell lung cancer.

Moxetumomab pasudotox, a first-in-class recombinant immunotoxin targeting CD22, produced deep and durable responses in a substantial proportion of pretreated patients with relapsed/refractory hairy cell leukemia.

First-line treatment with the oral AKT inhibitor ipatasertib shows a promising trend toward improving overall survival when added to paclitaxel for the treatment of locally advanced or metastatic triple-negative breast cancer.

Adding the CDK4/6 inhibitor ribociclib to fulvestrant significantly prolonged progression-free survival in postmenopausal women with hormone receptor-positive, HER2-negative advanced breast cancer who received no or 1 prior line of therapy.

Lenvatinib added to pembrolizumab demonstrated promising activity in patients with squamous cell carcinoma of the head and neck in an ongoing open-label phase Ib/II clinical trial.

The National Comprehensive Cancer Network has overhauled its guidelines for managing prostate cancer with a greater emphasis on risk stratification for molecular testing and therapy choices.

Specific guidance in the HIV-infected population was not previously available, partly because persons living with HIV were previously excluded from cancer clinical trials, creating a knowledge gap.

Antitumor activity of the combination of axitinib (Inlyta) and pembrolizumab (Keytruda) is superior to that expected from axitinib or PD-1/PD-L1 pathway inhibitor monotherapy in treatment-naïve patients with advanced renal cell carcinoma.

Cabozantinib (Cabometyx) improved progression-free survival as initial systemic therapy across subgroups of patients with intermediate- and poor-risk advanced RCC enrolled in the randomized phase II CABOSUN trial.
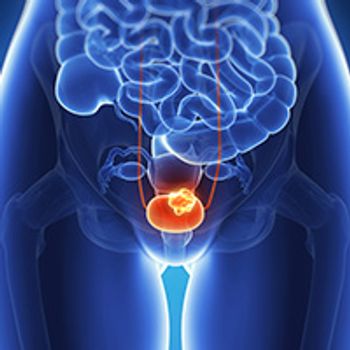
Erdafitinib showed responses in more than one-third of patients with pretreated metastatic or unresectable FGFR alteration-positive urothelial carcinoma.

Two-year follow-up data showed sustained improvements in overall survival with pembrolizumab over chemotherapy in pretreated patients with locally advanced or recurrent urothelial cancer.

Data from the first 13 evaluable patients enrolled in a phase II study of SM-88 showed a reduction in circulating tumor cells, a slowing of prostate-specific antigen increase, and delayed radiographic progression of disease in nonmetastatic prostate cancer.

The PARP inhibitor olaparib appeared to complement the antitumor activity of the PD-L1 inhibitor durvalumab in unselected men with metastatic castrate-resistant prostate cancer, according to findings from a phase II study presented at the 2018 Genitourinary Cancers Symposium.

Data from the CheckMate-142 study support the use of nivolumab (Opdivo) alone or in combination with ipilimumab (Yervoy) for the treatment of patients with previously treated DNA mismatch repair-deficient/microsatellite instability-high metastatic colorectal cancer.
Combining the investigational oral cancer stem cell pathway inhibitor napabucasin with the PD-1 inhibitor pembrolizumab showed a signal of efficacy in the first 8 patients enrolled in a multicenter phase I/II trial of patients with metastatic colorectal cancer.

Treatment with the PD-1 inhibitor pembrolizumab elicited promising progression-free survival and overall survival results in patients with advanced hepatocellular carcinoma who received previous treatment with sorafenib.
Combining lenvatinib (Lenvima) with PD-1 inhibitors had promising efficacy in patients with advanced intrahepatic cholangiocarcinoma, according to preliminary data from a single-center study.
Sequencing regorafenib before cetuximab showed superior overall survival compared with the reverse sequence in patients with metastatic colorectal cancer following failure of standard chemotherapy.

Nivolumab alone and in combination with ipilimumab induced responses in patients with heavily pretreated gastrointestinal stromal tumor.

Adding ramucirumab to standard first-line chemotherapy significantly improved investigator-assessed progression-free survival compared with chemotherapy plus placebo in treatment-naive patients with HER2-negative gastric cancer.

The novel investigational HER2-targeting antibody-drug conjugate trastuzumab deruxtecan showed promising antitumor activity in heavily pretreated patients with HER2-expressing gastric cancer.

An analysis of the phase III OlympiAD study showed that treatment discontinuation due to toxicity was less frequent with olaparib (Lynparza) monotherapy in patients with HER2-negative metastatic breast cancer and a germline BRCA mutation.

Selinexor combined with weekly bortezomib and low-dose dexamethasone produced rapid and durable responses in a dose escalation/expansion trial of patients with relapsed/refractory multiple myeloma.

Maintenance therapy with elotuzumab (Empliciti) and lenalidomide (Revlimid) after autologous stem cell transplant improves the quality of response achieved with induction therapy in patients with multiple myeloma.

Daratumumab (Darzalex) displayed single-agent activity in intermediate- and high-risk smoldering multiple myeloma, according to results from the phase II CENTAURUS study.

Despite a faster time to complete remission, the addition of rituximab (Rituxan) to ibrutinib (Imbruvica) did not improve PFS or overall survival OS compared with ibrutinib alone in patients with CLL.