
Monotherapy with an antibody drug conjugate targeting the transmembrane protein LIV-1 had encouraging antitumor activity in a phase 1 study of patients with heavily pretreated TNBC.

Your AI-Trained Oncology Knowledge Connection!


Monotherapy with an antibody drug conjugate targeting the transmembrane protein LIV-1 had encouraging antitumor activity in a phase 1 study of patients with heavily pretreated TNBC.

Enzalutamide (Xtandi) added to exemestane improved progression-free survival in patients with hormone receptor-positive advanced breast cancer and no prior endocrine therapy who were positive for a gene signature-based biomarker indicating androgen receptor-signaling.

Trastuzumab deruxtecan (ds-8201a), a HER2-targeting antibody-drug conjugate, demonstrated significant clinical activity in heavily pretreated patients with HER2-expressing metastatic breast cancers.

Substituting nab-paclitaxel (Abraxane) for solvent-based paclitaxel as neoadjuvant chemotherapy improved disease-free survival in patients with high-risk early breast cancer.

Defined composition CAR T cells directed against CD19 have potent anti-tumor activity in B cell malignancies, including acute lymphocytic leukemia.

After nearly 40 years with little in the way of drug development for the treatment of acute myeloid leukemia, four new drugs have been approved by the FDA in 2017 for AML, and several promising agents are in development.

The treatment approach for patients with relapsed/refractory multiple myeloma should be tailored based on biology of the disease, frailty of the patient, and comorbidities.

In relapsed classical Hodgkin lymphoma, the era of therapies post-brentuximab vedotin is developing rapidly.

Survival for patients with grade 1 to 2 follicular lymphoma is now measured in decades to coincide with improvements in therapy.
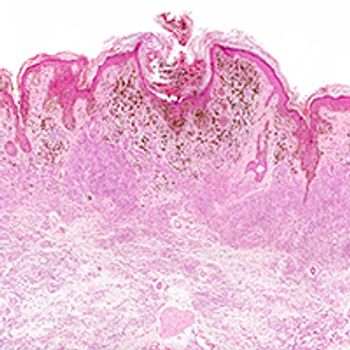
The neutrophil-to-lymphocyte ratio is an independent factor for overall survival in patients with metastatic melanoma, whether they receive targeted therapy or immunotherapy.
Cabozantinib and nivolumab with or without ipilimumab show activity in genitourinary tumors, particularly urothelial carcinoma, and have manageable safety profiles.

Nearly half of patients with resectable stage IIIB/C BRAF V600-mutant melanoma achieved pathologic complete response with neoadjuvant combination therapy consisting of dabrafenib (Tafinlar) and trametinib (Mekinist).

Pembrolizumab (Keytruda) reduced the risk of death compared with standard of care therapy in patients with relapsed/metastatic head and neck squamous cell carcinoma, but the difference fell just shy of statistical significance.

Nivolumab (Opdivo) may represent a new standard option for adjuvant therapy for patients with resected stage IIIB/C and IV melanoma, whether or not they have a BRAF mutation. In a comparison with current standard high-dose ipilimumab (Yervoy), nivolumab demonstrated a significant improvement in relapse-free survival.

The combination of nivolumab (Opdivo) and ipilimumab (Yervoy) was superior to sunitinib (Sutent) monotherapy as first-line treatment of advanced or metastatic renal cell carcinoma.

Ramucirumab (Cyramza) plus docetaxel improved progression-free survival over docetaxel alone in patients with advanced or metastatic urothelial cancer who have progressed on platinum-based chemotherapy.
Lenvatinib (Lenvima) combined with pembrolizumab (Keytruda) demonstrated promising antitumor activity in patients with metastatic clear cell renal cell carcinoma.

Two doses of nivolumab given about 1 month prior to surgery are well tolerated and reduces tumor size in about half of patients with squamous cell carcinoma of the head and neck.

Turning a nonimmunogenic (“cold”) tumor into an immunogenic (“hot”) tumor appears feasible in patients with metastatic triple negative breast cancer, thereby improving sensitivity to immune therapy with nivolumab.

Continuous treatment with nivolumab until disease progression was associated with superior progression-free survival compared with a 1-year fixed duration treatment for patients with previously treated advanced non-small cell lung cancer.

The anti-CD20 monoclonal antibody obinutuzumab (Gazyva) combined with bendamustine (Treanda; BG) in the frontline setting for patients with chronic lymphocytic leukemia was found to induce high rates of complete response and minimal residual disease negativity with no unexpected safety signals, according to results from a phase II open-label, multicenter study.

The future of treatment for ovarian cancer may lie in immunotherapy combinations with PARP inhibitors or checkpoint inhibitors.

Patients with T790M-positive non–small cell lung cancer had superior outcomes when treated with osimertinib (Tagrisso) for central nervous system metastases, according to phase III results presented at the 2017 ASCO Annual Meeting.
In follow-up results to data first presented in December 2016, investigators found that the combination of olaparib (Lynparza) and cediranib maleate continued to show superior progression-free survival compared with olaparib alone for women with BRCA-negative recurrent platinum-sensitive ovarian cancer.

Updates to the National Comprehensive Cancer Network guidelines for the management of advanced non–small cell lung cancer call for routine molecular analysis and testing for PD-L1 expression, preferably at diagnosis.

Updated guidelines for the management of invasive breast cancer, issued by the National Comprehensive Cancer Network, define indications for radiation therapy, the use of biomarkers and multigene assays in clinical decision making, and new concepts in endocrine therapy in early-stage and advanced-stage estrogen receptor-positive breast cancer.

Axicabtagene ciloleucel had an objective response rate of 76% and a complete response rate of 47% in patients with aggressive non-Hodgkin lymphoma followed for at least 1 month.
Vorinostat combined with tacrolimus and methotrexate represents a potentially effective combination to mitigate graft-versus-host disease in the setting of matched unrelated donor myeloablative conditioning hematopoietic stem cell transplant.

Proper care coordination and patient education are essential to the success of delivering chimeric antigen receptor T-cell therapy, particularly in preparing patients for potential adverse events.

A host of new and emerging therapies for acute and chronic graft-versus-host disease are on the horizon and include B-cell depletion, IL-2, inhibitors of JAK1/JAK2, extracorporeal photopheresis, and the BTK inhibitor ibrutinib.