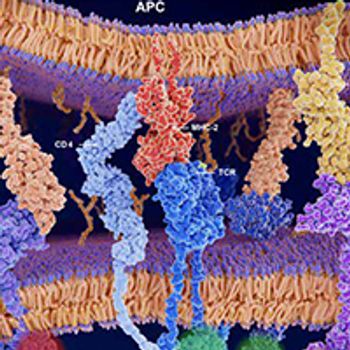
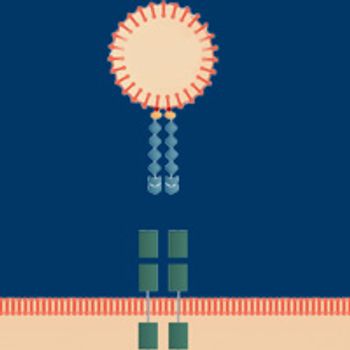
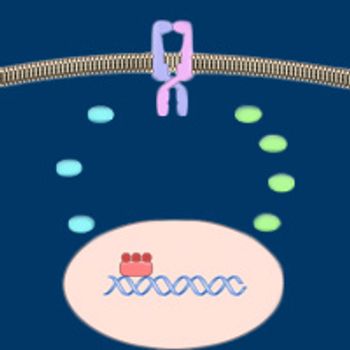
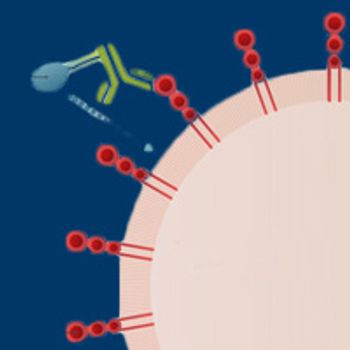
Over the past decade, immunotherapy has established itself as one of the pillars of cancer treatment, thanks in large part to the success of monoclonal antibodies that target the immune checkpoint protein PD-1 or its main ligand, PD-L1.

Your AI-Trained Oncology Knowledge Connection!

Over the past decade, immunotherapy has established itself as one of the pillars of cancer treatment, thanks in large part to the success of monoclonal antibodies that target the immune checkpoint protein PD-1 or its main ligand, PD-L1.
Investigators continue to find innovative ways to attack the WNT pathway beyond targeting the major molecular players.

The past 2 decades have been transformative for the treatment of non–small cell lung cancer; two-thirds of patients have been found to harbor molecular drivers, and a growing proportion of these are now targetable with FDA-approved drugs.
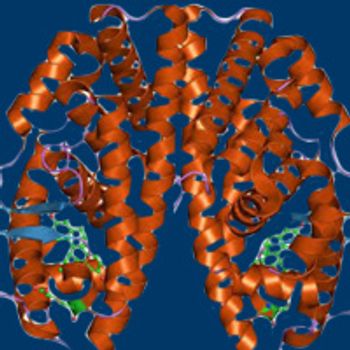
The approval of imatinib almost 20 years ago heralded the arrival of the targeted therapy era in oncology and thrust the ABL1 kinase into the limelight.
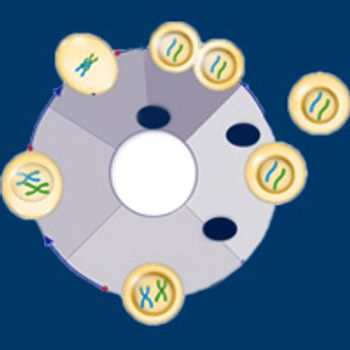
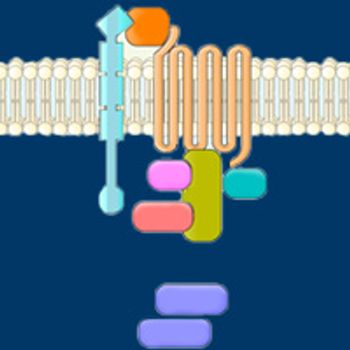
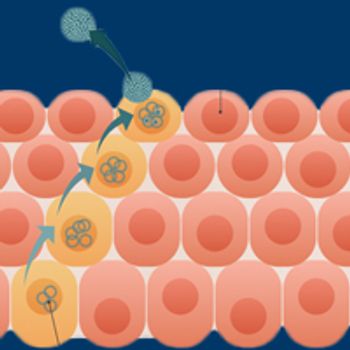
Serving as gatekeepers at the entry to the cell cycle, CDK4 and CDK6 make ideal therapeutic targets to block the unchecked proliferation that is a hallmark of cancer cells.
Despite being implicated across the spectrum of cancer hallmarks, aberrant AXL signaling is just starting to emerge as a distinct anticancer target, with a growing focus on specific inhibitors as well as alternative novel drug designs.

Investigators have turned their attention to B-cell maturation antigen, which offers an ideal target for multiple myeloma therapy because of its restricted expression pattern.

Adam D. Cohen, MD, discusses the prospects for BCMA-targeting options in multiple myeloma.
Results from a first-in-human study into ABBV-621, a TNF-related apoptosis-inducing ligand (TRAIL) receptor agonist, highlight the potential of focusing on TRAIL.
Daniel F. Hayes, MD, discusses the potential of liquid biopsies in breast and other cancers and highlights some major challenges that keep these tests from wider use.
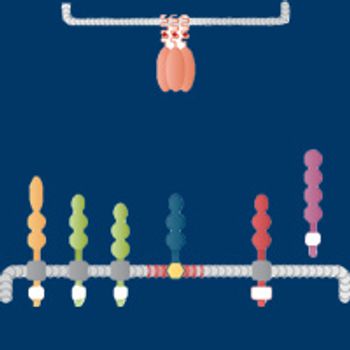
Despite a reasonable expectation that expression of HER3 and its ligand heregulin would be predictive biomarkers for HER3-targeted therapy, their usefulness in clinical trials has been hit-and-miss. Nevertheless, investigators have persevered, and new types of drugs have largely supplanted the first generation in clinical trials.

Although small molecule inhibitors of the Hedgehog signaling pathway have transformed the treatment paradigm for advanced basal cell carcinoma, the most common form of skin cancer, efforts to expand their use to other tumor types have proved elusive.

Liquid biopsy technologies have made substantial headway in recent years, sparking booming commercial interest in the development of potential clinical applications.

Allison Campbell, MD, PhD, discusses the synergy between immune checkpoint inhibitors and radiation therapy and the challenges facing ongoing clinical development.
A growing appreciation of the immunomodulatory properties of radiation therapy (RT) and their role in the rare, but highly sought-after “abscopal effect”—whereby localized RT elicits systemic antitumor effects—is fueling excitement in the radiation oncology field.
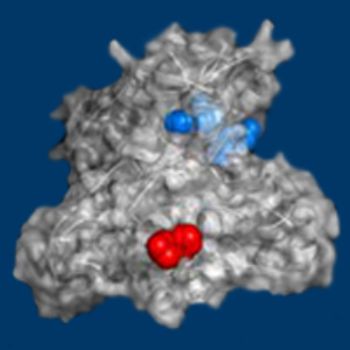
In the ongoing search for novel immunotherapies that might rival or surpass the efficacy of immune checkpoint inhibitors, drugs targeting IDO1—a key enzyme in tryptophan metabolism—have been a major focus in recent years.
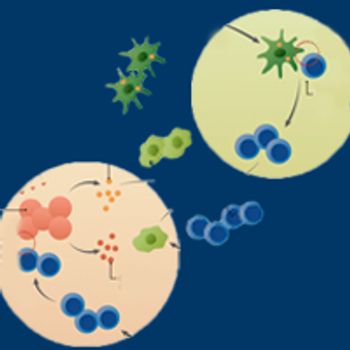
Immunotherapies designed to exploit the host immune system to specifically target cancer cells exploded onto the oncology scene in the mid-1980s, when the first such agents started to show success in melanoma and renal cell carcinoma.

Investigators are starting to make headway in their quest to develop therapies that counteract oncogenic mutations in the KRAS gene, a high-priority target in precision medicine that has long been deemed “undruggable.”
The development of therapeutic vaccines for patients with cancers associated with the human papillomavirus has emerged as a leading strategy in continuing research efforts to address the growing public health threat posed by the virus.
Despite the introduction of novel therapies over the past decade, advanced prostate cancer remains an incurable disease in need of new strategies to overcome drug resistance.

New strategies to address resistance in patients with estrogen receptor–positive breast cancer are in the works, thanks to a greater understanding of the cell-signaling networks activated during the course of disease.
Although hormonal manipulation was an established part of breast cancer treatment long before the underlying biology of the disease was characterized, advancements in the understanding of estrogen receptor signaling are rapidly changing the therapeutic landscape.

Although heritable mutations have been implicated in cancer risk, the role that these abberations play in the development of malignancies with acquired mutations is a question that will require studies of large data sets of patients.

Emerging findings from the most expansive studies of tumor genomes ever conducted are building a case for integrating all aspects of germline and somatic mutations into the analytical paradigm as a logical next step for precision oncology.
Named the medical invention of the Year by TIME magazine at the turn of the millennium, positron emission tomography/computed tomography has changed the landscape of cancer diagnosis, facilitating earlier detection and more accurate staging of a range of tumor types.
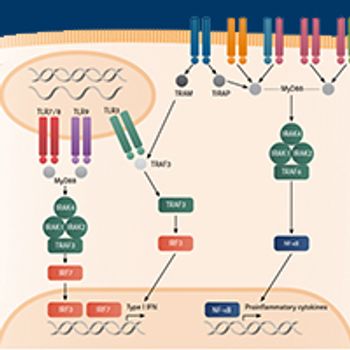
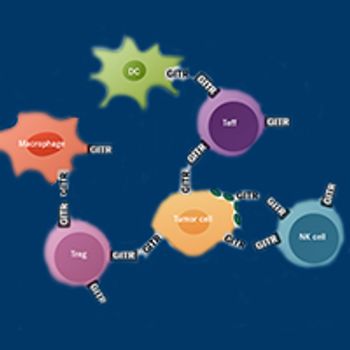
Toll-like receptors, a group of proteins that are components of innate immunity, are emerging as promising targets in a new wave of immunotherapies under development.

Cancer cells that manipulate the DNA damage response to foster the genomic instability that underlies many of their hallmark processes become heavily reliant on intact pathways for their survival, creating a targetable Achilles heel that can be exploited therapeutically.
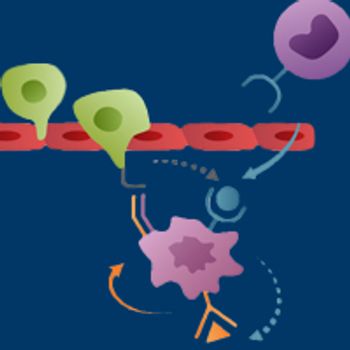
Chemokine receptor type 2, a major recruiter of circulating monocytes that subsequently develop into a protumoral type of macrophage within the tumor microenvironment, has emerged as a promising therapeutic target.
Thanks to technological advances, the past several decades have witnessed a blossoming appreciation of the varied composition of these microbial communities, their complex and dynamic relationship with the host, and the way they affect health and disease.
When it works, immunotherapy can dramatically outperform standard of care—for some cancer types, in ways thought unattainable a decade ago.